Interweave Implementation Guide - Local Development build (v0.1.0) built by the FHIR (HL7® FHIR® Standard) Build Tools. See the R4 profiles here.
Resource Profile: InterweaveEncounter
| Official URL: https://fhir.yhcr.nhs.uk/StructureDefinition/Interweave-Encounter | Version: 0.1.0 | |||
| Active as of 2024-07-17 | Computable Name: InterweaveEncounter | |||
Interweave Encounter resource profile.
Status: Active: Approved (STU)
Introduction
This profile sets minimum expectations for the Encounter resource.
The Encounter is a key resource - as it explains the who, where, when, and why of care that has been provided. Not only is the Encounter resource valuable in itself, but it also acts as a point of reference for linking to other clinical resources.
Its main use in our region at present is for acute care, where it can be used to describe inpatient, outpatient and emergency encounters.
As of this writing Encounters are not being used by Social Care - which instead uses a model based around the Episode of Care. See the Episode of Care profile for further details.
The Encounter is a complex FHIR Resource – and one which offers significant flexibility to support different representations. The FHIR guidance on anticipated usage is helpful and should be read as background, see https://www.hl7.org/fhir/STU3/encounter.html. As this states: “The expectation is that for each domain of exchange, profiles are used to limit the flexibility of Encounter to meet the demands of the use case”. Before looking at the data items in detail, it is therefore necessary to establish some overall guidelines on how the Encounter resource type will be used
Encounter Start/End
Whilst there is an intuitive understanding of what constitutes the start / end of an Encounter, it is challenging to establish a rigorous definition. Nevertheless, the following guidelines cover key points discussed to date:
-
An Encounter covers a period of continuous care
-
A change in care-setting constitutes a change of Encounter. (This would include moving from Emergency to Inpatient to Outpatient within a hospital – as indicated by the “class”)
-
A change in location within the same care setting does NOT constitute a change of Encounter. (For example moving between beds and/or wards within a hospital inpatient stay. This would instead be modelled using the “location” sub-structure of the Encounter)
-
Involvement of additional clinicians does NOT constitute a separate Encounter. For example, suppose a hospital inpatient is visited by a dietician during their stay:
- As a major contributor to the encounter the dietician would be referenced as one of the participants
- As a minor contributor the dietician would be referenced as the author of a CarePlan, performer of an Observation, or assessor of a ClinicalImpression. These in turn would be linked to the Encounter.
Encounter Structure and hierarchy
Any discussion of Encounters inevitably has to consider the topic of how Encounters are structured and grouped.
- The FHIR Encounter Resource includes the “partOf” field, which allows Encounters to be linked into structures and hierarchies.
- It is also possible to link to an Episode of Care
There is a need to balance the desire to accurately model the complexity of real-life vs the need to provide a simple model which is easy for Data Consumers to understand and to reliably display. Experience suggests that offering a plethora of varying complex hierarchical structures from different care settings makes the task of a Data Consumer extremely challenging.
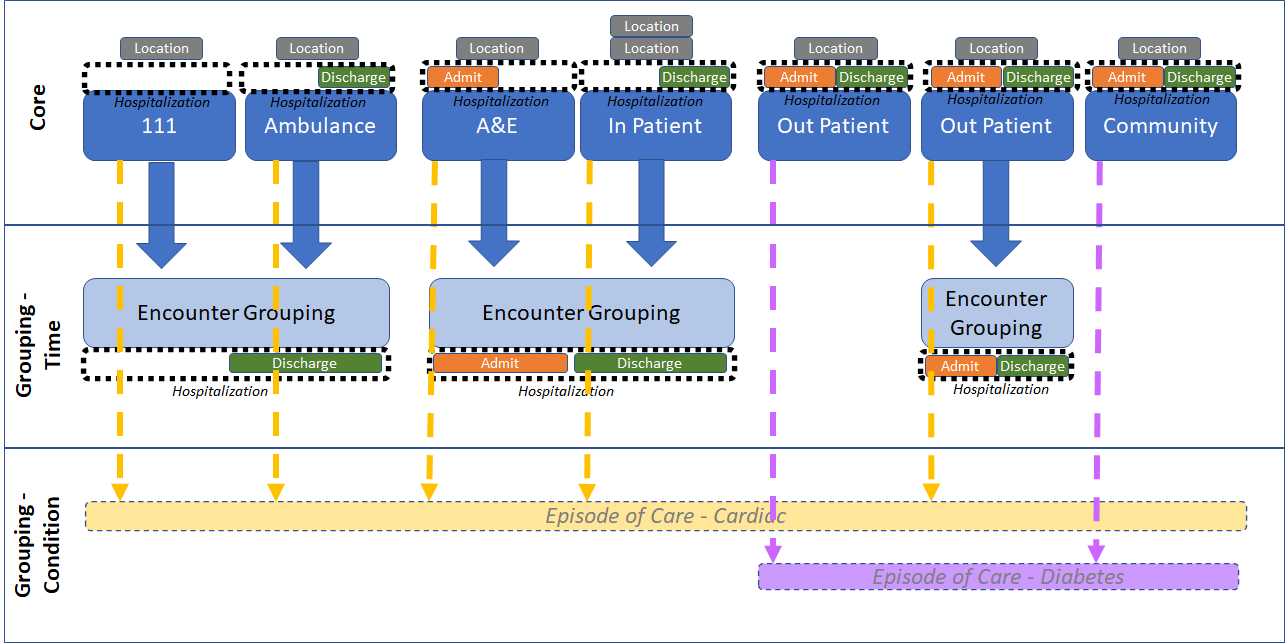
The core of the approach is therefore a simple flat list of Encounters. Two options are then offered to enrich this with different types of groupings:
-
Core Model - Simple flat list of Encounters
This is the basic model which all Data Providers and Consumers MUST support. It consists of a simple flat list of Encounters with no hierarchy whatsoever.
- Much of the value comes from this list and, for Direct Care purposes at least, it is not difficult for a clinician to look at the times and locations and deduce what has occurred.
- A important use-case is messaging-based consumers - eg Ambulance Transfer of Care and Subscription Notifications. These consumers see the world as a real-time stream of Encounter-based events. In this world-view it is difficult to comprehend hierarchy - and indeed the ultimate set of interrelationships may not even be known as the initial Encounter event unfolds. It is therefore extremely important that all of the necessary information can be conveyed as a “flat” stream of Encounter messages.
The basic model is therefore of standalone Encounters which have a full set of information populated to give a complete picture of what occurred.
A specific implication of this is in the use of the “hospitalization” structure which, despite the name, can be used to convey important admission and discharge information relevant to any care-setting:
- If the Encounter includes an Admission event, then the relevant portion of the hospitalization structure MUST be populated
- If the Encounter includes a Discharge event, then the relevant portion of the hospitalization structure MUST be populated
- Portions of the hospitalization structure which are irrelevant to this Encounter may be omitted.
- In other words, depending on circumstances, the hospitalization structure might be:
- Fully populated (for a simple standalone Encounter)
- Half populated (for an Encounter that is the first or last of a set)
- Not populated at all (more rarely, for an Encounter that is “in the middle” of a set)
-
Grouping Option 1 - Encounter Grouping (linking in time)
Despite the appeal of a simple flat list of Encounters, the concept of a “visit”, “hospitalisation”, or “incident” is widely recognised and agreed to be useful as a way of grouping Encounters that are linked in time. For example:
- An initial “emergency” visit to A&E is followed by admittance to the ward as an inpatient
- An initial call to 111 is followed by a visit at home from a first-responder, and finally a conveyance to hospital in an ambulance
A two-level hierarchy is therefore defined, based on the use of special type of Grouping Encounter to link together Encounters which comprise part of the same “visit”, “stay” or “incident”.
- A separate Encounter Grouping profile is provided to support this.
- Data Providers who feel it is relevant MAY provide this additional grouping information
- Data Consumers who are able MAY make use of this additional grouping information to provide a richer and more meaningful display to their users
In practical terms:
- The “partOf” field on the base Encounters is populated to point at a Grouping Encounter
- Only a SINGLE level of Encounter hierarchy is supported. The “partOf” field of a base Encounter must point ONLY at a single Grouping Encounter. Other more complex structures are NOT supported
- It is perfectly acceptable to have a Grouping Encounter which contains only a single base Encounter. In fact this is likely to be common - as when the initial encounter occurs it is not known how events will unfold. The simplest approach for a Maturity Level 2 Data Provider will therefore be to always create a Grouping Encounter in anticipation. With the grouping structure already in place, it becomes straightforward to add additional Encounters as-and-if they occur.
- It is, of course, also acceptable to have a standalone Encounter with no Grouping Encounter - for example where an Encounter is not going to be part of any grouping and this is known from the start.
- The Grouping Encounter is essentially an empty shell. Its purpose is purely to group. All of the important information is held in the base Encounters.
- The Grouping Encounter does however add value by capturing the overall period and the full set of “hospitalization” information about admission and discharge. Whilst this could be deduced from the base encounters, it is helpful and logical to also provide in one place here.
-
Grouping Option 2 - Episode of Care (linking by condition)
Another way of grouping Encounters goes beyond modelling a single visit or incident and links together a care pathway based on a Condition. This linkage is provided by the Episode of Care.
At first glance it can be difficult to distinguish an Encounter Grouping from an Episode of Care - however the FHIR specification provides helpful guidance, and in fact there are some clear differentiating features:
- An Episode of Care continues over a longer period of time. Specifically it can be used to link together multiple separate visits over a period of months or even years. For example an initial in-patient stay, and then several related out patient appointments, and then maybe another in-patient stay if there is a relapse.
-
An Episode of Care is based around a “condition” and is thus used to join-up a care pathway. Specifically, a patient with multiple conditions could have multiple Episodes of Care running concurrently. The Episode of Care is used to “pick out” from the mass of activity those Encounters relating to a particular care pathway. Therefore the Episode of Care MUST have its Condition field populated when using it to group Encounters in this way.
- The FHIR Specification states that an Episode of Care relates to a single organisation, and this is how we envisage it being used initially.
Longer term the definition of “organisation” might be considered a point of controversy, specifically is an Integrated Care System an “organisation”? This would provide a valuable mechanism to link up a cross-care-setting care pathway - noting that there is currently no obvious mechanism to identify and link encounters at this whole-system level. Extending an Episode of Care across multiple care settings in this way is therefore currently seen as aspiriational and unlikely to be implemented immediately. Please get in touch for further discussion if you believe you may be a first-of-type.
The diagram below summarises the above discussion - ie core Encounters, plus options for a single Grouping Encounter, and/or one or more Episodes of Care.
Encounters vs Appointments
Whilst the terms “Encounter” and “Appointment” might be used interchangeably in everyday speech, in FHIR they have specific meanings:
- An Appointment describes a plan for the future
- An Encounter generally describes something that is happening now, or has occurred in the past
In general therefore:
- An Appointment will lead to an Encounter - when the patient attends
- An Encounter may or may not come from an Appointment (ie scheduled vs unscheduled care)
The picture is further complicated as FHIR does allow an Encounter to be created with status “planned”, however this is not recommended here and should normally be represented instead with an Appointment.
Further useful guidance can be found on the FHIR website, here:
https://www.hl7.org/fhir/STU3/encounter.html#bnr
https://www.hl7.org/fhir/STU3/appointment.html#statuses
https://www.hl7.org/fhir/STU3/appointment.html#status-flow
Mandatory fields
A significant set of mandatory fields are defined in order to properly describe an Encounter:
-
Status - this is already mandatory in FHIR. As noted above the use of “planned” is discouraged - use Appointment instead for this.
-
Class - this provides a categorisation, ie Emergency, Inpatient, Ambulatory. This should always be known, and vital for meaningful display purposes. We have defined a custom code list which replicates the standard list provided by Care Connect, and adds a codes to identify an “Encounter Grouping”, and various types of ambulance/emergency service encounters. However it also enables the possibility of extending the list to cover a wider range of care settings if this is found to be necessary (please get in touch).
-
Subject - every encounter must be linked to a Patient (not a Group)
-
Participant - it is required to include EXACTLY ONE practitioner who has the “type” of “Primary Performer”. This should be the main person responsible - someone who it would be useful to contact if further information is desired. (If this person changed during the course of the encounter then please pick just ONE to finally hold this key role, and demote the others to “participant”)
Also included in the list of participants might be:
- Admitter and Discharger - should be included if known and relevant.
- Participant - FHIR offers a wealth of other participant type codes, however it is suggested that simply classifying others as “participant” is likely to be adequate in most cases.
Participants can be given a “period” and this is optional. For regional sharing the most important thing is to see who has been involved with the patient, rather than to construct a forensic timeline of involvements. However this information might be useful in the case of a long Encounter with many brief involvements, and so may be provided if desired.
-
Period When the encounter occurred is vital to know. The start date/time is always mandatory, but as per the FHIR specification, the end date/time may be omitted if the encounter is ongoing
Must Support fields
In addition the following fields are “Must Support” - ie they must be populated if relevant and known. These largely relate to providing additional “clinical” detail about the Encounter - including links to related FHIR Resources such as the originating Appointment, the Condition, etc. These build up the rich dataset around an Encounter and are important to provide, but may not yet be available for an initial Encounter implementation.
-
Identifier - a Local Id should be provided, such that could be quoted if manually getting in touch to find out more
- Type - categorises the type of place where the encounter took place. CareConnect modifies FHIR by providing a much more relevant list covering:
- Indirect encounters - eg phone, video, letter, etc
- In an establishment - a short list of top-level codes which cover a good range of care settings eg “Seen in clinic”, “Seen in own home”, “Seen in supervised accomodation”, etc.
- On the street
NB: The code for “Seen in Clinic” offers the ability to drill down into a long list of specific clinic types. However this overlaps to some extent with the purpose of the “Service Type” field - so it is sufficient here to populate simply “Seen in Clinic”.
-
Service Type (Extension) - this is perhaps one of the most important and useful fields about an Encounter as it describes the type of service - ie what the Encounter was “for”.
However this field is missing in FHIR STU3! This is corrected in FHIR R4, and so we pre-adopt it here as an extension.
We also pre-adopt the UKCore value set (based on SNOMED refset 1127531000000102: Services Simple Reference Set), which is more relevant than the default FHIR example and also covers social care
-
Priority: This provides useful information about whether it was emergency, routine, elective, etc
- Location - the location provides essential information about where the encounter took place. Exactly what is appropriate here will depend on the care setting:
- For a hospital information should be provided down to the “ward” level. Thus enabling a visitor to find the patient, as well as potentially giving some insight into the type of treatment being provided.
- For other (smaller) locations then the “site” level may be sufficient
- Other types of care (eg community, emergency) may take place at home or in a vehicle
It is useful to understand the history of where the patient has been seen, so the status and period MUST be populated, and a history SHOULD be provided. (As noted above, a change of location does not in itself constitute a new Encounter, simply append to this list).
-
Appointment: Link to the originating Appointment, if relevant
-
Reason: A long list of SNOMED codes to describe different reasons which may have led to the Encounter. (Note that this may duplicate to some extent information provided in a linked Appointment and/or Referral, but is seen as useful to pull through onto the Encounter itself also).
We pre-adopt the value set used in R4. This builds on the existing STU3 list covering SNOMED codes for “Clinical Finding” and “Procedure”, and adds codes for “Context-dependent categories” (Social Care) and “Events” (A&E)
-
Diagnosis: Link to a Condition diagnosed as a result of the Encounter. Can obviously be provided only if the Condition FHIR Resource is also being offered. If populated then it is required to rank the Conditions, and to assign one the “role” of “Chief Complaint”
- Outcome fields: Care Connect defines three extension fields which cover aspects of the encounter outcome:
- Outcome of Attendance - relevant to outpatient encounters
- Emergency Care Discharge Status - relevant to emergency encounters
- Discharge Method - found in the “hospitalization”, and relevant to inpatient encounters
These provide valuable information which is important to populate. However it is expected that only one of the three will be populated, as relevant for the type of encounter
- Emergency Care Discharge Destination - This extension has been added to record the discharge destination of patients which have attended ED. (based on SNOMED refset 999003011000000105: Emergency care discharge destination simple reference set)
-
Hospitalization: To provide details of admission and discharge. As described above then, depending on circumstances, it might be actually populated fully, partially, or not at all. See below for further details of the fields contained
- Status History - this is seen as important - to understand the timeline of the Encounter.
Optional fields
Other fields are optional and may be populated if known - on the understanding that not all data consumers will necessarily make use of them. Points of note include:
-
Part Of - as described above, this may be used to point to an overarching “EncounterGrouping” Encounter. No other complex structures or nesting are permitted.
-
Episode of Care - again as described above, this may be used to link up a care pathway by pointing to an Episode of Care.
-
Incoming Referral: Link to the originating Referral, if relevant and implemented. This could be very useful information. However FHIR makes significant changes from the STU3 “ReferralRequest” to the R4 “ServiceRequest”, and so we are reluctant to mandate implementation at this stage
-
Length - the period is already provided, so this may appear to be duplication. However it is encouraged to populate if possible as it is useful for analytic purposes. If provided then the duration SHOULD be in minutes, and should reflect the time the patient is receiving direct care - eg not including the time the patient is waiting to be seen in clinic. (This provides a further distinction and greater analytical accuracy over-and-above the “period”)
-
Encounter Transport - may be useful if relevant and known (however noting that it no longer exists in UK Core)
Discouraged or Removed fields
- Class History - as described in the introduction, a change of care setting would constitute a new Encounter. Therefore by definition an Encounter will only ever have a single Class.
- Account - for billing purposes, not relevant.
- Service Provider - duplicates information already available in the provenance tags
Hospitalization Structure
Within the Encounter sits the “Hospitalization” structure. This structure provides information about the admission and discharge. Therefore it is particularly important for a regional shared record - as this defines the touchpoints with other care providers.
Fields in the Hospitalization structure are as follows:
- Must Support
- Admission Method - this CareConnect extension provides a useful list of codes about the method of admission (eg Planned, A&E, transfer, etc)
- Discharge Method - this CareConnect extension provides a useful list of codes about the method of discharge relevant to an inpatient stay (eg clinical discharge, self-discharge, deceased, etc). It is one of three alternatives for providing outcome information, depending on the type of encounter - see above under the main encounter “must support” heading for further details.
- Origin - Information about the location which the patient arrived from (if relevant / known)
- Required at the “site” level if arriving from another institution
- Optional if arriving from a residential address
-
Admit Source - Useful information about the type of place the patient came from (eg home, other NHS hospital, care home, etc)
- Please note that the NHS Data Dictionary national codes for Source of Admission has been replaced with Admission Source. The current Valueset contains codes from both codesystems, however please use the new Interweave code system for new data provision projects.
- Destination - Information about the location which the patient is discharged to (if relevant / known)
- Required at the “site” level if discharged to another institution
- Optional if discharged to a residential address
- Discharge Disposition - Useful information about the type of place the patient has been discharged to (eg home, other NHS hospital, care home, etc). (We use a value set which updates that provided by CareConnect with the latest improved list from the NHS Data Dictionary)
- Medically Safe For Discharge - This extension has been added to capture important information to assist with discharge planning and analysis. It contains a status code (ready, not ready, or unknown), plus the predicted and actual date when the patient is medically safe for discharge.
Note that Origin and Destination are likely to be external locations - please refer to guidance on the Location profile about use of References. For example the use of a Contained Resource may be appropriate.
- Optional
- Readmission - flag may be provided if known and relevant
- Discouraged
- Diet Preferences, Special Courtesy, Special Arrangement - additional details that are relevant internally for planning the patient’s stay, but not so relevant for external sharing.
Usage:
- Examples for this Resource Profile: Encounter/InterweaveEncounterExample-MaturityLevel1, Encounter/InterweaveEncounterExample-MaturityLevel2-Part1 and Encounter/InterweaveEncounterExample-MaturityLevel2-Part2
Formal Views of Profile Content
Description of Profiles, Differentials, Snapshots and how the different presentations work.
This structure is derived from CareConnect-Encounter-1
| Name | Flags | Card. | Type | Description & Constraints |
|---|---|---|---|---|
 | 0..* | CareConnect-Encounter-1 | An interaction during which services are provided to the patient | |
  | S | 0..1 | id | Logical id of this artifact |
  | ||||
   | S | 0..1 | id | Version specific identifier |
   | S | 0..1 | instant | MANDATORY except in Contained Resources. When the resource version last changed. |
   | S | 0..* | uri | Profiles this resource claims to conform to. Should list (i) this profile (ii) underlying CareConnect profile |
   | 0..* | Coding | DISCOURAGED - may not be honoured by Data Consumers | |
   | 0..* | Coding | Tags applied to this resource Slice: Unordered, Open by value:system | |
    | S | 0..1 | Coding | MANDATORY except in Contained Resources. The Data Provider Id (and display text) of the system supplying the data |
     | 1..1 | uri | Identity of the terminology system Fixed Value: https://yhcr.nhs.uk/Source | |
     | S | 1..1 | code | The Data Provider Id of the system supplying the data |
     | S | 1..1 | string | Name of the system supplying the data |
    | S | 0..1 | Coding | MANDATORY except in Contained Resources. The ODS Code (and display text) of the organisation responsible for the data |
     | 1..1 | uri | Identity of the terminology system Fixed Value: https://yhcr.nhs.uk/Provenance | |
     | S | 1..1 | code | The ODS Code of the organisation responsible for the data |
     | S | 1..1 | string | Name of the organisation supplying the data |
  | 0..1 | uri | DISCOURAGED - may not be honoured by Data Consumers | |
  | 0..1 | code | English is assumed (not currently a multi-lingual implementation) | |
  | 0..1 | Narrative | DISCOURAGED - the preferred approach is to offer structured data fields which a Data Consumer can then render and present in a manner most suited to its users | |
  | S | 0..1 | Extension-CareConnect-OutcomeOfAttendance-1 | An extension to the Encounter resource to record the outcome of an Out-Patient attendance. |
  | S | 0..1 | Extension-CareConnect-EmergencyCareDischargeStatus-1 | An extension to the Encounter resource which is used indicate the status of the Patient on discharge from an Emergency Care Department. |
  | S | 0..1 | CodeableConcept | Discharge destination of patients which have attended ED. URL: https://fhir.yhcr.nhs.uk/StructureDefinition/Extension-Interweave-EDDischargeDestination Binding: Interweave ED Discharge Destination (preferred) |
  | S | 0..1 | CodeableConcept | Specific type of service (pre-adopted from R4) URL: https://fhir.yhcr.nhs.uk/StructureDefinition/Extension-Interweave-R4EncounterServiceType Binding: Interweave UkCore Care Setting Type (preferred) |
  | 0..* | Identifier | Identifier(s) by which this encounter is known Slice: Unordered, Open by value:system | |
   | S | 0..1 | Identifier | Identifier(s) by which this encounter is known |
    | S | 1..1 | uri | The namespace for the identifier value Fixed Value: https://fhir.yhcr.nhs.uk/Id/local-encounter-identifier |
    | S | 1..1 | string | The Local encounter Identifier. Please prefix with ODS code plus period (XXX.) to ensure unique |
    | 0..0 | |||
  | S | 1..1 | code | arrived | triaged | in-progress | onleave | finished | cancelled + (Note: 'planned' is also possible, but normally represented instead as an Appointment) |
  | S | 0..* | BackboneElement | List of past encounter statuses |
  | S | 1..1 | Coding | Classification of the encounter. EXTENSIBLE on request, eg to cover other care settings Binding: InterweaveEncounterClass (required) |
   | 1..1 | uri | Identity of the terminology system | |
   | 1..1 | code | Symbol in syntax defined by the system | |
   | 1..1 | string | Representation defined by the system | |
  | 0..0 | |||
  | S | 0..1 | CodeableConcept | Specific type of encounter Binding: Care Connect Encounter Type (required) |
   | 1..1 | Coding | Code defined by a terminology system | |
    | 1..1 | uri | Identity of the terminology system | |
    | 1..1 | code | Symbol in syntax defined by the system | |
    | 1..1 | string | Representation defined by the system | |
   | S | 1..* | Coding | Code defined by a terminology system Binding: Care Connect Encounter Type (required) |
  | S | 0..1 | CodeableConcept | Indicates the urgency of the encounter Binding: InterweaveEncounterPriority (required) |
   | ||||
    | 1..1 | uri | Identity of the terminology system | |
    | 1..1 | code | Symbol in syntax defined by the system | |
    | 1..1 | string | Representation defined by the system | |
  | S | 1..1 | Reference(CareConnectPatient1) | The patient (NOT group) present at the encounter |
   | 1..1 | string | Reference to a resource (could be Contained) | |
   | 0..1 | Identifier | If relevant could include an id | |
   | 1..1 | string | Description of the referenced resource | |
  | ||||
   | 1..1 | string | Reference to a resource (could be Contained) | |
   | 0..1 | Identifier | If relevant could include an id | |
   | 0..1 | string | If relevant, description of the referenced resource | |
  | S | 1..* | BackboneElement | List of participants involved in the encounter |
   | S | 1..1 | CodeableConcept | Role of participant in encounter Binding: ParticipantType (required) |
    | ||||
     | 1..1 | uri | Identity of the terminology system | |
     | 1..1 | code | Symbol in syntax defined by the system | |
     | 1..1 | string | Representation defined by the system | |
   | S | 1..1 | Reference(CareConnect-Practitioner-1) | Persons involved in the encounter other than the patient |
    | 1..1 | string | Reference to a resource (could be Contained) | |
    | 0..1 | Identifier | If relevant could include an id | |
    | 1..1 | string | Description of the referenced resource | |
  | S | 0..1 | Reference(Appointment) | The appointment that scheduled this encounter |
   | 1..1 | string | Reference to a resource (could be Contained) | |
   | 0..1 | Identifier | If relevant could include an id | |
   | 0..1 | string | If relevant, description of the referenced resource | |
  | S | 1..1 | Period | The start and end time of the encounter |
   | S | 1..1 | dateTime | Starting time with inclusive boundary |
   | S | 0..1 | dateTime | End time with inclusive boundary, if not ongoing |
  | 0..1 | Duration | Quantity of time the encounter lasted (less time absent). Please use minutes. | |
  | S | 0..* | CodeableConcept | Reason the encounter takes place (code) Binding: Interweave R4 Encounter Reason (preferred) |
   | 0..* | Coding | Code defined by a terminology system | |
    | 1..1 | uri | Identity of the terminology system | |
    | 1..1 | code | Symbol in syntax defined by the system | |
    | 1..1 | string | Representation defined by the system | |
  | S | 0..* | BackboneElement | The list of diagnosis relevant to this encounter Slice: Unordered, Open by value:role |
   | Content/Rules for all slices | |||
    | S | 1..1 | Reference(CareConnect-Condition-1) | Reason the encounter takes place (resource) |
     | 1..1 | string | Reference to a resource (could be Contained) | |
     | 0..1 | Identifier | If relevant could include an id | |
     | 0..1 | string | If relevant, description of the referenced resource | |
    | S | 1..1 | CodeableConcept | Role that this diagnosis has within the encounter (e.g. admission, billing, discharge …) Binding: DiagnosisRole (required) |
     | ||||
      | 1..1 | uri | Identity of the terminology system | |
      | 1..1 | code | Symbol in syntax defined by the system | |
      | 1..1 | string | Representation defined by the system | |
    | S | 1..1 | positiveInt | Ranking of the diagnosis (for each role type) |
   | S | 0..1 | BackboneElement | The list of diagnosis relevant to this encounter |
    | 0..1 | CodeableConcept | Role that this diagnosis has within the encounter (e.g. admission, billing, discharge …) Fixed Value: As shown | |
     | 1..1 | Coding | Code defined by a terminology system Fixed Value: (complex) | |
      | 1..1 | uri | Identity of the terminology system Fixed Value: http://hl7.org/fhir/diagnosis-role | |
      | 1..1 | code | Symbol in syntax defined by the system Fixed Value: CC | |
      | 1..1 | string | Representation defined by the system Fixed Value: Chief complaint | |
  | 0..0 | |||
  | S | 0..1 | BackboneElement | Details about the admission to a healthcare service |
   | S | 0..1 | Extension-CareConnect-AdmissionMethod-1 | An extension to the Encounter resource to record how a Patient was admitted to hospital. |
   | S | 0..1 | Extension-CareConnect-DischargeMethod-1 | An extension to the Encounter resource to record the method of discharge from hospital. |
   | S | 0..1 | (Complex) | Medically Safe for Discharge URL: https://fhir.yhcr.nhs.uk/StructureDefinition/Extension-Interweave-MedicallySafeForDischarge |
   | 0..1 | Reference(CareConnect-Location-1) | The location from which the patient came before admission. Useful to provide if possible, in particular to reference a 'site' if transfered from another institution. | |
    | 1..1 | string | Reference to a resource (could be Contained) | |
    | 0..1 | Identifier | If relevant could include an id | |
    | 1..1 | string | Description of the referenced resource | |
   | S | 0..1 | CodeableConcept | From where patient was admitted (physician referral, transfer) Binding: Interweave Admission Source codes (required) |
    | ||||
     | 1..1 | uri | Identity of the terminology system | |
     | 1..1 | code | Symbol in syntax defined by the system | |
     | 1..1 | string | Representation defined by the system | |
   | 0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing | |
   | 0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing | |
   | 0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing | |
   | S | 0..1 | Reference(CareConnect-Location-1) | Location to which the patient is discharged. Important to provide if known to support discharge planning, and/or to reference a 'site' if transfered to another institution. |
    | 1..1 | string | Reference to a resource (could be Contained) | |
    | 0..1 | Identifier | If relevant could include an id | |
    | 1..1 | string | Description of the referenced resource | |
   | S | 0..1 | CodeableConcept | Category or kind of location after discharge Binding: Interweave Discharge Destination codes (required) |
    | ||||
     | 1..1 | uri | Identity of the terminology system | |
     | 1..1 | code | Symbol in syntax defined by the system | |
     | 1..1 | string | Representation defined by the system | |
  | S | 0..* | BackboneElement | Location the encounter takes place (at Ward level) |
   | S | 1..1 | Reference(CareConnect-Location-1) | Location the encounter takes place |
    | 1..1 | string | Reference to a resource (could be Contained) | |
    | 0..1 | Identifier | If relevant could include an id | |
    | 1..1 | string | Description of the referenced resource | |
   | S | 1..1 | code | planned | active | reserved | completed |
   | S | 1..1 | Period | Time period during which the patient was present at the location |
  | 0..1 | Reference(CareConnect-Organization-1) | DISCOURAGED: This is instead covered via the provenance tags | |
  | 0..1 | Reference(InterweaveEncounterGrouping) | Another Encounter this encounter is part of | |
   | 1..1 | string | Reference to a resource (could be Contained) | |
   | 0..1 | Identifier | If relevant could include an id | |
   | 0..1 | string | If relevant, description of the referenced resource | |
 Documentation for this format Documentation for this format | ||||
Terminology Bindings (Differential)
| Path | Conformance | ValueSet |
| Encounter.class | required | InterweaveEncounterClass |
| Encounter.type | required | Care Connect Encounter Type |
| Encounter.type.coding:snomedCT | required | Care Connect Encounter Type |
| Encounter.priority | required | InterweaveEncounterPriority |
| Encounter.participant.type | required | ParticipantType |
| Encounter.reason | preferred | Interweave R4 Encounter Reason |
| Encounter.diagnosis.role | required | DiagnosisRole |
| Encounter.hospitalization.admitSource | required | Interweave Admission Source codes |
| Encounter.hospitalization.dischargeDisposition | required | Interweave Discharge Destination codes |
| Name | Flags | Card. | Type | Description & Constraints | ||||
|---|---|---|---|---|---|---|---|---|
 | 0..* | CareConnect-Encounter-1 | An interaction during which services are provided to the patient | |||||
  | SΣ | 0..1 | id | Logical id of this artifact | ||||
  | Σ | 0..1 | Meta | Metadata about the resource | ||||
   | SΣ | 0..1 | id | Version specific identifier | ||||
   | SΣ | 0..1 | instant | MANDATORY except in Contained Resources. When the resource version last changed. | ||||
   | SΣ | 0..* | uri | Profiles this resource claims to conform to. Should list (i) this profile (ii) underlying CareConnect profile | ||||
   | Σ | 0..* | Coding | DISCOURAGED - may not be honoured by Data Consumers Binding: All Security Labels (extensible): Security Labels from the Healthcare Privacy and Security Classification System. | ||||
   | Σ | 0..* | Coding | Tags applied to this resource Slice: Unordered, Open by value:system Binding: Common Tags (example): Codes that represent various types of tags, commonly workflow-related; e.g. "Needs review by Dr. Jones" | ||||
    | SΣ | 0..1 | Coding | MANDATORY except in Contained Resources. The Data Provider Id (and display text) of the system supplying the data Binding: Common Tags (example): Codes that represent various types of tags, commonly workflow-related; e.g. "Needs review by Dr. Jones" | ||||
     | Σ | 1..1 | uri | Identity of the terminology system Fixed Value: https://yhcr.nhs.uk/Source | ||||
     | SΣ | 1..1 | code | The Data Provider Id of the system supplying the data | ||||
     | SΣ | 1..1 | string | Name of the system supplying the data | ||||
    | SΣ | 0..1 | Coding | MANDATORY except in Contained Resources. The ODS Code (and display text) of the organisation responsible for the data Binding: Common Tags (example): Codes that represent various types of tags, commonly workflow-related; e.g. "Needs review by Dr. Jones" | ||||
     | Σ | 1..1 | uri | Identity of the terminology system Fixed Value: https://yhcr.nhs.uk/Provenance | ||||
     | SΣ | 1..1 | code | The ODS Code of the organisation responsible for the data | ||||
     | SΣ | 1..1 | string | Name of the organisation supplying the data | ||||
  | ?!Σ | 0..1 | uri | DISCOURAGED - may not be honoured by Data Consumers | ||||
  | 0..1 | code | English is assumed (not currently a multi-lingual implementation) Binding: Common Languages (extensible): A human language.
| |||||
  | 0..1 | Narrative | DISCOURAGED - the preferred approach is to offer structured data fields which a Data Consumer can then render and present in a manner most suited to its users | |||||
  | 0..1 | (Complex) | Encounter transport URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-CareConnect-EncounterTransport-1 | |||||
  | S | 0..1 | CodeableConcept | An extension to the Encounter resource to record the outcome of an Out-Patient attendance. URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-CareConnect-OutcomeOfAttendance-1 Binding: NHS Data Model and Dictionary Outcome Of Attendance (required): This records the outcome of an Out-Patient Attendance Consultant. | ||||
  | S | 0..1 | CodeableConcept | An extension to the Encounter resource which is used indicate the status of the Patient on discharge from an Emergency Care Department. URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-CareConnect-EmergencyCareDischargeStatus-1 Binding: Care Connect Emergency Care Discharge Status (required): The status of the Patient on discharge from an Emergency Care Department. | ||||
  | S | 0..1 | CodeableConcept | Discharge destination of patients which have attended ED. URL: https://fhir.yhcr.nhs.uk/StructureDefinition/Extension-Interweave-EDDischargeDestination Binding: Interweave ED Discharge Destination (preferred) | ||||
  | S | 0..1 | CodeableConcept | Specific type of service (pre-adopted from R4) URL: https://fhir.yhcr.nhs.uk/StructureDefinition/Extension-Interweave-R4EncounterServiceType Binding: Interweave UkCore Care Setting Type (preferred) | ||||
  | ?! | 0..* | Extension | Extensions that cannot be ignored | ||||
  | Σ | 0..* | Identifier | Identifier(s) by which this encounter is known Slice: Unordered, Open by value:system | ||||
   | Content/Rules for all slices | |||||||
    | ?!Σ | 0..1 | code | usual | official | temp | secondary (If known) Binding: IdentifierUse (required): Identifies the purpose for this identifier, if known . | ||||
    | Σ | 1..1 | uri | The namespace for the identifier value Example General: http://www.acme.com/identifiers/patient | ||||
    | Σ | 1..1 | string | The value that is unique Example General: 123456 | ||||
   | SΣ | 0..1 | Identifier | Identifier(s) by which this encounter is known | ||||
    | ?!Σ | 0..1 | code | usual | official | temp | secondary (If known) Binding: IdentifierUse (required): Identifies the purpose for this identifier, if known . | ||||
    | SΣ | 1..1 | uri | The namespace for the identifier value Fixed Value: https://fhir.yhcr.nhs.uk/Id/local-encounter-identifier | ||||
    | SΣ | 1..1 | string | The Local encounter Identifier. Please prefix with ODS code plus period (XXX.) to ensure unique Example General: 123456 | ||||
  | ?!SΣ | 1..1 | code | arrived | triaged | in-progress | onleave | finished | cancelled + (Note: 'planned' is also possible, but normally represented instead as an Appointment) Binding: EncounterStatus (required): Current state of the encounter | ||||
  | S | 0..* | BackboneElement | List of past encounter statuses | ||||
   | ?!Σ | 0..* | Extension | Extensions that cannot be ignored | ||||
   | 1..1 | code | planned | arrived | triaged | in-progress | onleave | finished | cancelled + Binding: EncounterStatus (required): Current state of the encounter | |||||
   | 1..1 | Period | The time that the episode was in the specified status | |||||
  | SΣ | 1..1 | Coding | Classification of the encounter. EXTENSIBLE on request, eg to cover other care settings Binding: InterweaveEncounterClass (required) | ||||
   | Σ | 1..1 | uri | Identity of the terminology system | ||||
   | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
   | Σ | 1..1 | string | Representation defined by the system | ||||
  | SΣ | 0..1 | CodeableConcept | Specific type of encounter Binding: Care Connect Encounter Type (required) | ||||
   | Σ | 1..1 | Coding | Code defined by a terminology system Slice: Unordered, Open by value:system | ||||
    | Content/Rules for all slices | |||||||
     | Σ | 1..1 | uri | Identity of the terminology system | ||||
     | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
     | Σ | 1..1 | string | Representation defined by the system | ||||
    | SΣ | 1..* | Coding | Code defined by a terminology system Binding: Care Connect Encounter Type (required) | ||||
     | 0..* | (Complex) | The SNOMED CT Description ID for the display URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-coding-sctdescid | |||||
     | Σ | 1..1 | uri | Identity of the terminology system Fixed Value: http://snomed.info/sct | ||||
     | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
     | Σ | 1..1 | string | Representation defined by the system | ||||
  | S | 0..1 | CodeableConcept | Indicates the urgency of the encounter Binding: InterweaveEncounterPriority (required) | ||||
  | SΣ | 1..1 | Reference(CareConnectPatient1) | The patient (NOT group) present at the encounter | ||||
   | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
   | Σ | 0..1 | Identifier | If relevant could include an id | ||||
   | Σ | 1..1 | string | Description of the referenced resource | ||||
  | SΣ | 1..* | BackboneElement | List of participants involved in the encounter | ||||
   | ?!Σ | 0..* | Extension | Extensions that cannot be ignored | ||||
   | SΣ | 1..1 | CodeableConcept | Role of participant in encounter Binding: ParticipantType (required) | ||||
   | SΣ | 1..1 | Reference(CareConnect-Practitioner-1) | Persons involved in the encounter other than the patient | ||||
    | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    | Σ | 0..1 | Identifier | If relevant could include an id | ||||
    | Σ | 1..1 | string | Description of the referenced resource | ||||
  | SΣ | 0..1 | Reference(Appointment) | The appointment that scheduled this encounter | ||||
   | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
   | Σ | 0..1 | Identifier | If relevant could include an id | ||||
   | Σ | 0..1 | string | If relevant, description of the referenced resource | ||||
  | S | 1..1 | Period | The start and end time of the encounter | ||||
   | SΣC | 1..1 | dateTime | Starting time with inclusive boundary | ||||
   | SΣC | 0..1 | dateTime | End time with inclusive boundary, if not ongoing | ||||
  | 0..1 | Duration | Quantity of time the encounter lasted (less time absent). Please use minutes. | |||||
  | SΣ | 0..* | CodeableConcept | Reason the encounter takes place (code) Binding: Interweave R4 Encounter Reason (preferred) | ||||
   | Σ | 0..* | Coding | Code defined by a terminology system Slice: Unordered, Open by value:system | ||||
    | Content/Rules for all slices | |||||||
     | Σ | 1..1 | uri | Identity of the terminology system | ||||
     | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
     | Σ | 1..1 | string | Representation defined by the system | ||||
    | Σ | 0..1 | Coding | Code defined by a terminology system | ||||
     | 0..* | (Complex) | The SNOMED CT Description ID for the display URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-coding-sctdescid | |||||
     | Σ | 1..1 | uri | Identity of the terminology system Fixed Value: http://snomed.info/sct | ||||
     | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
     | Σ | 1..1 | string | Representation defined by the system | ||||
  | SΣ | 0..* | BackboneElement | The list of diagnosis relevant to this encounter Slice: Unordered, Open by value:role | ||||
   | Content/Rules for all slices | |||||||
    | ?!Σ | 0..* | Extension | Extensions that cannot be ignored | ||||
    | S | 1..1 | Reference(CareConnect-Condition-1) | Reason the encounter takes place (resource) | ||||
     | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
     | Σ | 0..1 | Identifier | If relevant could include an id | ||||
     | Σ | 0..1 | string | If relevant, description of the referenced resource | ||||
    | S | 1..1 | CodeableConcept | Role that this diagnosis has within the encounter (e.g. admission, billing, discharge …) Binding: DiagnosisRole (required) | ||||
    | S | 1..1 | positiveInt | Ranking of the diagnosis (for each role type) | ||||
   | SΣ | 0..1 | BackboneElement | The list of diagnosis relevant to this encounter | ||||
    | ?!Σ | 0..* | Extension | Extensions that cannot be ignored | ||||
    | 1..1 | Reference(CareConnect-Procedure-1 | CareConnect-Condition-1) | Reason the encounter takes place (resource) | |||||
    | 0..1 | CodeableConcept | Role that this diagnosis has within the encounter (e.g. admission, billing, discharge …) Binding: DiagnosisRole (preferred): The type of diagnosis this condition represents Fixed Value: As shown | |||||
     | 0..0 | string | xml:id (or equivalent in JSON) | |||||
     | 0..0 | Extension | Additional Content defined by implementations | |||||
     | 1..1 | Coding | Code defined by a terminology system Fixed Value: (complex) | |||||
      | 0..0 | string | xml:id (or equivalent in JSON) | |||||
      | 0..0 | Extension | Additional Content defined by implementations | |||||
      | 1..1 | uri | Identity of the terminology system Fixed Value: http://hl7.org/fhir/diagnosis-role | |||||
      | 0..0 | string | Version of the system - if relevant | |||||
      | 1..1 | code | Symbol in syntax defined by the system Fixed Value: CC | |||||
      | 1..1 | string | Representation defined by the system Fixed Value: Chief complaint | |||||
      | 0..0 | boolean | If this coding was chosen directly by the user | |||||
     | 0..0 | string | Plain text representation of the concept | |||||
  | S | 0..1 | BackboneElement | Details about the admission to a healthcare service | ||||
   | S | 0..1 | CodeableConcept | An extension to the Encounter resource to record how a Patient was admitted to hospital. URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-CareConnect-AdmissionMethod-1 Binding: NHS Data Model and Dictionary Admission Method (required): The method of admission to a Hospital Provider Spell. | ||||
   | S | 0..1 | CodeableConcept | An extension to the Encounter resource to record the method of discharge from hospital. URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-CareConnect-DischargeMethod-1 Binding: NHS Data Model and Dictionary Discharge Method (required): The method of discharge from a Hospital Provider Spell. | ||||
   | S | 0..1 | (Complex) | Medically Safe for Discharge URL: https://fhir.yhcr.nhs.uk/StructureDefinition/Extension-Interweave-MedicallySafeForDischarge | ||||
   | ?!Σ | 0..* | Extension | Extensions that cannot be ignored | ||||
   | 0..1 | Reference(CareConnect-Location-1) | The location from which the patient came before admission. Useful to provide if possible, in particular to reference a 'site' if transfered from another institution. | |||||
    | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    | Σ | 0..1 | Identifier | If relevant could include an id | ||||
    | Σ | 1..1 | string | Description of the referenced resource | ||||
   | S | 0..1 | CodeableConcept | From where patient was admitted (physician referral, transfer) Binding: Interweave Admission Source codes (required) | ||||
   | 0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing Binding: Diet (extensible) | |||||
   | 0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing Binding: SpecialCourtesy (preferred): Special courtesies | |||||
   | 0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing Binding: SpecialArrangements (preferred): Special arrangements | |||||
   | S | 0..1 | Reference(CareConnect-Location-1) | Location to which the patient is discharged. Important to provide if known to support discharge planning, and/or to reference a 'site' if transfered to another institution. | ||||
    | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    | Σ | 0..1 | Identifier | If relevant could include an id | ||||
    | Σ | 1..1 | string | Description of the referenced resource | ||||
   | S | 0..1 | CodeableConcept | Category or kind of location after discharge Binding: Interweave Discharge Destination codes (required) | ||||
  | S | 0..* | BackboneElement | Location the encounter takes place (at Ward level) | ||||
   | ?!Σ | 0..* | Extension | Extensions that cannot be ignored | ||||
   | S | 1..1 | Reference(CareConnect-Location-1) | Location the encounter takes place | ||||
    | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    | Σ | 0..1 | Identifier | If relevant could include an id | ||||
    | Σ | 1..1 | string | Description of the referenced resource | ||||
   | S | 1..1 | code | planned | active | reserved | completed Binding: EncounterLocationStatus (required): The status of the location. | ||||
   | S | 1..1 | Period | Time period during which the patient was present at the location | ||||
  | 0..1 | Reference(CareConnect-Organization-1) | DISCOURAGED: This is instead covered via the provenance tags | |||||
  | 0..1 | Reference(InterweaveEncounterGrouping) | Another Encounter this encounter is part of | |||||
   | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
   | Σ | 0..1 | Identifier | If relevant could include an id | ||||
   | Σ | 0..1 | string | If relevant, description of the referenced resource | ||||
 Documentation for this format Documentation for this format | ||||||||
Terminology Bindings
| Path | Conformance | ValueSet / Code | ||||
| Encounter.meta.security | extensible | All Security Labels | ||||
| Encounter.meta.tag | example | Common Tags | ||||
| Encounter.meta.tag:Source | example | Common Tags | ||||
| Encounter.meta.tag:Provenance | example | Common Tags | ||||
| Encounter.language | extensible | Common Languages
| ||||
| Encounter.identifier.use | required | IdentifierUse | ||||
| Encounter.identifier:localIdentifier.use | required | IdentifierUse | ||||
| Encounter.status | required | EncounterStatus | ||||
| Encounter.statusHistory.status | required | EncounterStatus | ||||
| Encounter.class | required | InterweaveEncounterClass | ||||
| Encounter.classHistory.class | extensible | ActEncounterCode | ||||
| Encounter.type | required | Care Connect Encounter Type | ||||
| Encounter.type.coding:snomedCT | required | Care Connect Encounter Type | ||||
| Encounter.priority | required | InterweaveEncounterPriority | ||||
| Encounter.participant.type | required | ParticipantType | ||||
| Encounter.reason | preferred | Interweave R4 Encounter Reason | ||||
| Encounter.diagnosis.role | required | DiagnosisRole | ||||
| Encounter.diagnosis:chiefComplaint.role | preferred | Fixed Value: CC("Chief complaint") | ||||
| Encounter.hospitalization.admitSource | required | Interweave Admission Source codes | ||||
| Encounter.hospitalization.dietPreference | extensible | Diet | ||||
| Encounter.hospitalization.specialCourtesy | preferred | SpecialCourtesy | ||||
| Encounter.hospitalization.specialArrangement | preferred | SpecialArrangements | ||||
| Encounter.hospitalization.dischargeDisposition | required | Interweave Discharge Destination codes | ||||
| Encounter.location.status | required | EncounterLocationStatus |
Constraints
| Id | Grade | Path(s) | Details | Requirements |
| dom-1 | error | Encounter | If the resource is contained in another resource, it SHALL NOT contain any narrative : contained.text.empty() | |
| dom-2 | error | Encounter | If the resource is contained in another resource, it SHALL NOT contain nested Resources : contained.contained.empty() | |
| dom-3 | error | Encounter | If the resource is contained in another resource, it SHALL be referred to from elsewhere in the resource : contained.where(('#'+id in %resource.descendants().reference).not()).empty() | |
| dom-4 | error | Encounter | If a resource is contained in another resource, it SHALL NOT have a meta.versionId or a meta.lastUpdated : contained.meta.versionId.empty() and contained.meta.lastUpdated.empty() | |
| ele-1 | error | Encounter.extension:encounterTransport, Encounter.extension:outcomeOfAttendance, Encounter.extension:emergencyCareDischargeStatus, Encounter.statusHistory, Encounter.participant, Encounter.diagnosis, Encounter.diagnosis:chiefComplaint, Encounter.hospitalization, Encounter.hospitalization.extension:admissionMethod, Encounter.hospitalization.extension:dischargeMethod, Encounter.location | All FHIR elements must have a @value or children : hasValue() | (children().count() > id.count()) | |
| ext-1 | error | Encounter.extension:encounterTransport, Encounter.extension:outcomeOfAttendance, Encounter.extension:emergencyCareDischargeStatus, Encounter.hospitalization.extension:admissionMethod, Encounter.hospitalization.extension:dischargeMethod | Must have either extensions or value[x], not both : extension.exists() != value.exists() |
| Name | Flags | Card. | Type | Description & Constraints | ||||
|---|---|---|---|---|---|---|---|---|
 | 0..* | CareConnect-Encounter-1 | An interaction during which services are provided to the patient | |||||
  | SΣ | 0..1 | id | Logical id of this artifact | ||||
  | Σ | 0..1 | Meta | Metadata about the resource | ||||
   | 0..1 | string | xml:id (or equivalent in JSON) | |||||
   | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
   | SΣ | 0..1 | id | Version specific identifier | ||||
   | SΣ | 0..1 | instant | MANDATORY except in Contained Resources. When the resource version last changed. | ||||
   | SΣ | 0..* | uri | Profiles this resource claims to conform to. Should list (i) this profile (ii) underlying CareConnect profile | ||||
   | Σ | 0..* | Coding | DISCOURAGED - may not be honoured by Data Consumers Binding: All Security Labels (extensible): Security Labels from the Healthcare Privacy and Security Classification System. | ||||
   | Σ | 0..* | Coding | Tags applied to this resource Slice: Unordered, Open by value:system Binding: Common Tags (example): Codes that represent various types of tags, commonly workflow-related; e.g. "Needs review by Dr. Jones" | ||||
    | SΣ | 0..1 | Coding | MANDATORY except in Contained Resources. The Data Provider Id (and display text) of the system supplying the data Binding: Common Tags (example): Codes that represent various types of tags, commonly workflow-related; e.g. "Needs review by Dr. Jones" | ||||
     | 0..1 | string | xml:id (or equivalent in JSON) | |||||
     | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
     | Σ | 1..1 | uri | Identity of the terminology system Fixed Value: https://yhcr.nhs.uk/Source | ||||
     | Σ | 0..1 | string | Version of the system - if relevant | ||||
     | SΣ | 1..1 | code | The Data Provider Id of the system supplying the data | ||||
     | SΣ | 1..1 | string | Name of the system supplying the data | ||||
     | Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
    | SΣ | 0..1 | Coding | MANDATORY except in Contained Resources. The ODS Code (and display text) of the organisation responsible for the data Binding: Common Tags (example): Codes that represent various types of tags, commonly workflow-related; e.g. "Needs review by Dr. Jones" | ||||
     | 0..1 | string | xml:id (or equivalent in JSON) | |||||
     | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
     | Σ | 1..1 | uri | Identity of the terminology system Fixed Value: https://yhcr.nhs.uk/Provenance | ||||
     | Σ | 0..1 | string | Version of the system - if relevant | ||||
     | SΣ | 1..1 | code | The ODS Code of the organisation responsible for the data | ||||
     | SΣ | 1..1 | string | Name of the organisation supplying the data | ||||
     | Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
  | ?!Σ | 0..1 | uri | DISCOURAGED - may not be honoured by Data Consumers | ||||
  | 0..1 | code | English is assumed (not currently a multi-lingual implementation) Binding: Common Languages (extensible): A human language.
| |||||
  | 0..1 | Narrative | DISCOURAGED - the preferred approach is to offer structured data fields which a Data Consumer can then render and present in a manner most suited to its users | |||||
  | 0..* | Resource | Contained, inline Resources | |||||
  | 0..* | Extension | Extension Slice: Unordered, Open by value:url | |||||
  | 0..1 | (Complex) | Encounter transport URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-CareConnect-EncounterTransport-1 | |||||
  | S | 0..1 | CodeableConcept | An extension to the Encounter resource to record the outcome of an Out-Patient attendance. URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-CareConnect-OutcomeOfAttendance-1 Binding: NHS Data Model and Dictionary Outcome Of Attendance (required): This records the outcome of an Out-Patient Attendance Consultant. | ||||
  | S | 0..1 | CodeableConcept | An extension to the Encounter resource which is used indicate the status of the Patient on discharge from an Emergency Care Department. URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-CareConnect-EmergencyCareDischargeStatus-1 Binding: Care Connect Emergency Care Discharge Status (required): The status of the Patient on discharge from an Emergency Care Department. | ||||
  | S | 0..1 | CodeableConcept | Discharge destination of patients which have attended ED. URL: https://fhir.yhcr.nhs.uk/StructureDefinition/Extension-Interweave-EDDischargeDestination Binding: Interweave ED Discharge Destination (preferred) | ||||
  | S | 0..1 | CodeableConcept | Specific type of service (pre-adopted from R4) URL: https://fhir.yhcr.nhs.uk/StructureDefinition/Extension-Interweave-R4EncounterServiceType Binding: Interweave UkCore Care Setting Type (preferred) | ||||
  | ?! | 0..* | Extension | Extensions that cannot be ignored | ||||
  | Σ | 0..* | Identifier | Identifier(s) by which this encounter is known Slice: Unordered, Open by value:system | ||||
   | Content/Rules for all slices | |||||||
    | 0..1 | string | xml:id (or equivalent in JSON) | |||||
    | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
    | ?!Σ | 0..1 | code | usual | official | temp | secondary (If known) Binding: IdentifierUse (required): Identifies the purpose for this identifier, if known . | ||||
    | Σ | 0..1 | CodeableConcept | Description of identifier Binding: Identifier Type Codes (extensible): A coded type for an identifier that can be used to determine which identifier to use for a specific purpose. | ||||
    | Σ | 1..1 | uri | The namespace for the identifier value Example General: http://www.acme.com/identifiers/patient | ||||
    | Σ | 1..1 | string | The value that is unique Example General: 123456 | ||||
    | Σ | 0..1 | Period | Time period when id is/was valid for use | ||||
    | Σ | 0..1 | Reference(CareConnect-Organization-1) | Organization that issued id (may be just text) | ||||
   | SΣ | 0..1 | Identifier | Identifier(s) by which this encounter is known | ||||
    | 0..1 | string | xml:id (or equivalent in JSON) | |||||
    | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
    | ?!Σ | 0..1 | code | usual | official | temp | secondary (If known) Binding: IdentifierUse (required): Identifies the purpose for this identifier, if known . | ||||
    | Σ | 0..1 | CodeableConcept | Description of identifier Binding: Identifier Type Codes (extensible): A coded type for an identifier that can be used to determine which identifier to use for a specific purpose. | ||||
    | SΣ | 1..1 | uri | The namespace for the identifier value Fixed Value: https://fhir.yhcr.nhs.uk/Id/local-encounter-identifier | ||||
    | SΣ | 1..1 | string | The Local encounter Identifier. Please prefix with ODS code plus period (XXX.) to ensure unique Example General: 123456 | ||||
    | Σ | 0..1 | Reference(CareConnect-Organization-1) | Organization that issued id (may be just text) | ||||
  | ?!SΣ | 1..1 | code | arrived | triaged | in-progress | onleave | finished | cancelled + (Note: 'planned' is also possible, but normally represented instead as an Appointment) Binding: EncounterStatus (required): Current state of the encounter | ||||
  | S | 0..* | BackboneElement | List of past encounter statuses | ||||
   | 0..1 | string | xml:id (or equivalent in JSON) | |||||
   | 0..* | Extension | Additional Content defined by implementations | |||||
   | ?!Σ | 0..* | Extension | Extensions that cannot be ignored | ||||
   | 1..1 | code | planned | arrived | triaged | in-progress | onleave | finished | cancelled + Binding: EncounterStatus (required): Current state of the encounter | |||||
   | 1..1 | Period | The time that the episode was in the specified status | |||||
  | SΣ | 1..1 | Coding | Classification of the encounter. EXTENSIBLE on request, eg to cover other care settings Binding: InterweaveEncounterClass (required) | ||||
   | 0..1 | string | xml:id (or equivalent in JSON) | |||||
   | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
   | Σ | 1..1 | uri | Identity of the terminology system | ||||
   | Σ | 0..1 | string | Version of the system - if relevant | ||||
   | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
   | Σ | 1..1 | string | Representation defined by the system | ||||
   | Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
  | SΣ | 0..1 | CodeableConcept | Specific type of encounter Binding: Care Connect Encounter Type (required) | ||||
   | 0..1 | string | xml:id (or equivalent in JSON) | |||||
   | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
   | Σ | 1..1 | Coding | Code defined by a terminology system Slice: Unordered, Open by value:system | ||||
    | Content/Rules for all slices | |||||||
     | 0..1 | string | xml:id (or equivalent in JSON) | |||||
     | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
     | Σ | 1..1 | uri | Identity of the terminology system | ||||
     | Σ | 0..1 | string | Version of the system - if relevant | ||||
     | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
     | Σ | 1..1 | string | Representation defined by the system | ||||
     | Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
    | SΣ | 1..* | Coding | Code defined by a terminology system Binding: Care Connect Encounter Type (required) | ||||
     | 0..1 | string | xml:id (or equivalent in JSON) | |||||
     | 0..* | Extension | Extension Slice: Unordered, Open by value:url | |||||
     | 0..* | (Complex) | The SNOMED CT Description ID for the display URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-coding-sctdescid | |||||
     | Σ | 1..1 | uri | Identity of the terminology system Fixed Value: http://snomed.info/sct | ||||
     | Σ | 0..1 | string | Version of the system - if relevant | ||||
     | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
     | Σ | 1..1 | string | Representation defined by the system | ||||
     | Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
   | Σ | 0..1 | string | Plain text representation of the concept | ||||
  | S | 0..1 | CodeableConcept | Indicates the urgency of the encounter Binding: InterweaveEncounterPriority (required) | ||||
   | 0..1 | string | xml:id (or equivalent in JSON) | |||||
   | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
   | Σ | 0..* | Coding | Code defined by a terminology system | ||||
    | 0..1 | string | xml:id (or equivalent in JSON) | |||||
    | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
    | Σ | 1..1 | uri | Identity of the terminology system | ||||
    | Σ | 0..1 | string | Version of the system - if relevant | ||||
    | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
    | Σ | 1..1 | string | Representation defined by the system | ||||
    | Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
   | Σ | 0..1 | string | Plain text representation of the concept | ||||
  | SΣ | 1..1 | Reference(CareConnectPatient1) | The patient (NOT group) present at the encounter | ||||
   | 0..1 | string | xml:id (or equivalent in JSON) | |||||
   | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
   | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
   | Σ | 0..1 | Identifier | If relevant could include an id | ||||
   | Σ | 1..1 | string | Description of the referenced resource | ||||
  | Σ | 0..* | Reference(EpisodeOfCare) | Episode(s) of care that this encounter should be recorded against | ||||
  | 0..* | Reference(ReferralRequest) | The ReferralRequest that initiated this encounter | |||||
   | 0..1 | string | xml:id (or equivalent in JSON) | |||||
   | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
   | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
   | Σ | 0..1 | Identifier | If relevant could include an id | ||||
   | Σ | 0..1 | string | If relevant, description of the referenced resource | ||||
  | SΣ | 1..* | BackboneElement | List of participants involved in the encounter | ||||
   | 0..1 | string | xml:id (or equivalent in JSON) | |||||
   | 0..* | Extension | Additional Content defined by implementations | |||||
   | ?!Σ | 0..* | Extension | Extensions that cannot be ignored | ||||
   | SΣ | 1..1 | CodeableConcept | Role of participant in encounter Binding: ParticipantType (required) | ||||
    | 0..1 | string | xml:id (or equivalent in JSON) | |||||
    | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
    | Σ | 0..* | Coding | Code defined by a terminology system | ||||
     | 0..1 | string | xml:id (or equivalent in JSON) | |||||
     | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
     | Σ | 1..1 | uri | Identity of the terminology system | ||||
     | Σ | 0..1 | string | Version of the system - if relevant | ||||
     | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
     | Σ | 1..1 | string | Representation defined by the system | ||||
     | Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
    | Σ | 0..1 | string | Plain text representation of the concept | ||||
   | 0..1 | Period | Period of time during the encounter that the participant participated | |||||
   | SΣ | 1..1 | Reference(CareConnect-Practitioner-1) | Persons involved in the encounter other than the patient | ||||
    | 0..1 | string | xml:id (or equivalent in JSON) | |||||
    | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
    | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    | Σ | 0..1 | Identifier | If relevant could include an id | ||||
    | Σ | 1..1 | string | Description of the referenced resource | ||||
  | SΣ | 0..1 | Reference(Appointment) | The appointment that scheduled this encounter | ||||
   | 0..1 | string | xml:id (or equivalent in JSON) | |||||
   | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
   | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
   | Σ | 0..1 | Identifier | If relevant could include an id | ||||
   | Σ | 0..1 | string | If relevant, description of the referenced resource | ||||
  | S | 1..1 | Period | The start and end time of the encounter | ||||
   | 0..1 | string | xml:id (or equivalent in JSON) | |||||
   | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
   | SΣC | 1..1 | dateTime | Starting time with inclusive boundary | ||||
   | SΣC | 0..1 | dateTime | End time with inclusive boundary, if not ongoing | ||||
  | 0..1 | Duration | Quantity of time the encounter lasted (less time absent). Please use minutes. | |||||
  | SΣ | 0..* | CodeableConcept | Reason the encounter takes place (code) Binding: Interweave R4 Encounter Reason (preferred) | ||||
   | 0..1 | string | xml:id (or equivalent in JSON) | |||||
   | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
   | Σ | 0..* | Coding | Code defined by a terminology system Slice: Unordered, Open by value:system | ||||
    | Content/Rules for all slices | |||||||
     | 0..1 | string | xml:id (or equivalent in JSON) | |||||
     | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
     | Σ | 1..1 | uri | Identity of the terminology system | ||||
     | Σ | 0..1 | string | Version of the system - if relevant | ||||
     | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
     | Σ | 1..1 | string | Representation defined by the system | ||||
     | Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
    | Σ | 0..1 | Coding | Code defined by a terminology system | ||||
     | 0..1 | string | xml:id (or equivalent in JSON) | |||||
     | 0..* | Extension | Extension Slice: Unordered, Open by value:url | |||||
     | 0..* | (Complex) | The SNOMED CT Description ID for the display URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-coding-sctdescid | |||||
     | Σ | 1..1 | uri | Identity of the terminology system Fixed Value: http://snomed.info/sct | ||||
     | Σ | 0..1 | string | Version of the system - if relevant | ||||
     | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
     | Σ | 1..1 | string | Representation defined by the system | ||||
     | Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
   | Σ | 0..1 | string | Plain text representation of the concept | ||||
  | SΣ | 0..* | BackboneElement | The list of diagnosis relevant to this encounter Slice: Unordered, Open by value:role | ||||
   | Content/Rules for all slices | |||||||
    | 0..1 | string | xml:id (or equivalent in JSON) | |||||
    | 0..* | Extension | Additional Content defined by implementations | |||||
    | ?!Σ | 0..* | Extension | Extensions that cannot be ignored | ||||
    | S | 1..1 | Reference(CareConnect-Condition-1) | Reason the encounter takes place (resource) | ||||
     | 0..1 | string | xml:id (or equivalent in JSON) | |||||
     | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
     | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
     | Σ | 0..1 | Identifier | If relevant could include an id | ||||
     | Σ | 0..1 | string | If relevant, description of the referenced resource | ||||
    | S | 1..1 | CodeableConcept | Role that this diagnosis has within the encounter (e.g. admission, billing, discharge …) Binding: DiagnosisRole (required) | ||||
     | 0..1 | string | xml:id (or equivalent in JSON) | |||||
     | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
     | Σ | 0..* | Coding | Code defined by a terminology system | ||||
      | 0..1 | string | xml:id (or equivalent in JSON) | |||||
      | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
      | Σ | 1..1 | uri | Identity of the terminology system | ||||
      | Σ | 0..1 | string | Version of the system - if relevant | ||||
      | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
      | Σ | 1..1 | string | Representation defined by the system | ||||
      | Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
     | Σ | 0..1 | string | Plain text representation of the concept | ||||
    | S | 1..1 | positiveInt | Ranking of the diagnosis (for each role type) | ||||
   | SΣ | 0..1 | BackboneElement | The list of diagnosis relevant to this encounter | ||||
    | 0..1 | string | xml:id (or equivalent in JSON) | |||||
    | 0..* | Extension | Additional Content defined by implementations | |||||
    | ?!Σ | 0..* | Extension | Extensions that cannot be ignored | ||||
    | 1..1 | Reference(CareConnect-Procedure-1 | CareConnect-Condition-1) | Reason the encounter takes place (resource) | |||||
    | 0..1 | CodeableConcept | Role that this diagnosis has within the encounter (e.g. admission, billing, discharge …) Binding: DiagnosisRole (preferred): The type of diagnosis this condition represents Fixed Value: As shown | |||||
     | 0..0 | string | xml:id (or equivalent in JSON) | |||||
     | 0..0 | Extension | Additional Content defined by implementations | |||||
     | 1..1 | Coding | Code defined by a terminology system Fixed Value: (complex) | |||||
      | 0..0 | string | xml:id (or equivalent in JSON) | |||||
      | 0..0 | Extension | Additional Content defined by implementations | |||||
      | 1..1 | uri | Identity of the terminology system Fixed Value: http://hl7.org/fhir/diagnosis-role | |||||
      | 0..0 | string | Version of the system - if relevant | |||||
      | 1..1 | code | Symbol in syntax defined by the system Fixed Value: CC | |||||
      | 1..1 | string | Representation defined by the system Fixed Value: Chief complaint | |||||
      | 0..0 | boolean | If this coding was chosen directly by the user | |||||
     | 0..0 | string | Plain text representation of the concept | |||||
    | 0..1 | positiveInt | Ranking of the diagnosis (for each role type) | |||||
  | S | 0..1 | BackboneElement | Details about the admission to a healthcare service | ||||
   | 0..1 | string | xml:id (or equivalent in JSON) | |||||
   | 0..* | Extension | Extension Slice: Unordered, Open by value:url | |||||
   | S | 0..1 | CodeableConcept | An extension to the Encounter resource to record how a Patient was admitted to hospital. URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-CareConnect-AdmissionMethod-1 Binding: NHS Data Model and Dictionary Admission Method (required): The method of admission to a Hospital Provider Spell. | ||||
   | S | 0..1 | CodeableConcept | An extension to the Encounter resource to record the method of discharge from hospital. URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-CareConnect-DischargeMethod-1 Binding: NHS Data Model and Dictionary Discharge Method (required): The method of discharge from a Hospital Provider Spell. | ||||
   | S | 0..1 | (Complex) | Medically Safe for Discharge URL: https://fhir.yhcr.nhs.uk/StructureDefinition/Extension-Interweave-MedicallySafeForDischarge | ||||
   | ?!Σ | 0..* | Extension | Extensions that cannot be ignored | ||||
   | 0..1 | Identifier | Pre-admission identifier | |||||
    | 0..1 | string | xml:id (or equivalent in JSON) | |||||
    | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
    | ?!Σ | 0..1 | code | usual | official | temp | secondary (If known) Binding: IdentifierUse (required): Identifies the purpose for this identifier, if known . | ||||
    | Σ | 0..1 | CodeableConcept | Description of identifier Binding: Identifier Type Codes (extensible): A coded type for an identifier that can be used to determine which identifier to use for a specific purpose. | ||||
    | Σ | 1..1 | uri | The namespace for the identifier value Example General: http://www.acme.com/identifiers/patient | ||||
    | Σ | 1..1 | string | The value that is unique Example General: 123456 | ||||
    | Σ | 0..1 | Period | Time period when id is/was valid for use | ||||
    | Σ | 0..1 | Reference(CareConnect-Organization-1) | Organization that issued id (may be just text) | ||||
   | 0..1 | Reference(CareConnect-Location-1) | The location from which the patient came before admission. Useful to provide if possible, in particular to reference a 'site' if transfered from another institution. | |||||
    | 0..1 | string | xml:id (or equivalent in JSON) | |||||
    | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
    | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    | Σ | 0..1 | Identifier | If relevant could include an id | ||||
    | Σ | 1..1 | string | Description of the referenced resource | ||||
   | S | 0..1 | CodeableConcept | From where patient was admitted (physician referral, transfer) Binding: Interweave Admission Source codes (required) | ||||
    | 0..1 | string | xml:id (or equivalent in JSON) | |||||
    | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
    | Σ | 0..* | Coding | Code defined by a terminology system | ||||
     | 0..1 | string | xml:id (or equivalent in JSON) | |||||
     | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
     | Σ | 1..1 | uri | Identity of the terminology system | ||||
     | Σ | 0..1 | string | Version of the system - if relevant | ||||
     | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
     | Σ | 1..1 | string | Representation defined by the system | ||||
     | Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
    | Σ | 0..1 | string | Plain text representation of the concept | ||||
   | 0..1 | CodeableConcept | The type of hospital re-admission that has occurred (if any). If the value is absent, then this is not identified as a readmission Binding: v2 Re-Admission Indicator (example): The reason for re-admission of this hospitalization encounter. | |||||
    | 0..1 | string | xml:id (or equivalent in JSON) | |||||
    | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
    | Σ | 0..* | Coding | Code defined by a terminology system Slice: Unordered, Open by value:system | ||||
     | Σ | 0..1 | Coding | Code defined by a terminology system | ||||
      | 0..1 | string | xml:id (or equivalent in JSON) | |||||
      | 0..* | Extension | Extension Slice: Unordered, Open by value:url | |||||
      | 0..* | (Complex) | The SNOMED CT Description ID for the display URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-coding-sctdescid | |||||
      | Σ | 1..1 | uri | Identity of the terminology system Fixed Value: http://snomed.info/sct | ||||
      | Σ | 0..1 | string | Version of the system - if relevant | ||||
      | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
      | Σ | 1..1 | string | Representation defined by the system | ||||
      | Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
    | Σ | 0..1 | string | Plain text representation of the concept | ||||
   | 0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing Binding: Diet (extensible) | |||||
   | 0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing Binding: SpecialCourtesy (preferred): Special courtesies | |||||
   | 0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing Binding: SpecialArrangements (preferred): Special arrangements | |||||
   | S | 0..1 | Reference(CareConnect-Location-1) | Location to which the patient is discharged. Important to provide if known to support discharge planning, and/or to reference a 'site' if transfered to another institution. | ||||
    | 0..1 | string | xml:id (or equivalent in JSON) | |||||
    | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
    | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    | Σ | 0..1 | Identifier | If relevant could include an id | ||||
    | Σ | 1..1 | string | Description of the referenced resource | ||||
   | S | 0..1 | CodeableConcept | Category or kind of location after discharge Binding: Interweave Discharge Destination codes (required) | ||||
    | 0..1 | string | xml:id (or equivalent in JSON) | |||||
    | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
    | Σ | 0..* | Coding | Code defined by a terminology system | ||||
     | 0..1 | string | xml:id (or equivalent in JSON) | |||||
     | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
     | Σ | 1..1 | uri | Identity of the terminology system | ||||
     | Σ | 0..1 | string | Version of the system - if relevant | ||||
     | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
     | Σ | 1..1 | string | Representation defined by the system | ||||
     | Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
    | Σ | 0..1 | string | Plain text representation of the concept | ||||
  | S | 0..* | BackboneElement | Location the encounter takes place (at Ward level) | ||||
   | 0..1 | string | xml:id (or equivalent in JSON) | |||||
   | 0..* | Extension | Additional Content defined by implementations | |||||
   | ?!Σ | 0..* | Extension | Extensions that cannot be ignored | ||||
   | S | 1..1 | Reference(CareConnect-Location-1) | Location the encounter takes place | ||||
    | 0..1 | string | xml:id (or equivalent in JSON) | |||||
    | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
    | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    | Σ | 0..1 | Identifier | If relevant could include an id | ||||
    | Σ | 1..1 | string | Description of the referenced resource | ||||
   | S | 1..1 | code | planned | active | reserved | completed Binding: EncounterLocationStatus (required): The status of the location. | ||||
   | S | 1..1 | Period | Time period during which the patient was present at the location | ||||
  | 0..1 | Reference(CareConnect-Organization-1) | DISCOURAGED: This is instead covered via the provenance tags | |||||
  | 0..1 | Reference(InterweaveEncounterGrouping) | Another Encounter this encounter is part of | |||||
   | 0..1 | string | xml:id (or equivalent in JSON) | |||||
   | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
   | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
   | Σ | 0..1 | Identifier | If relevant could include an id | ||||
   | Σ | 0..1 | string | If relevant, description of the referenced resource | ||||
 Documentation for this format Documentation for this format | ||||||||
Terminology Bindings
| Path | Conformance | ValueSet / Code | ||||
| Encounter.meta.security | extensible | All Security Labels | ||||
| Encounter.meta.tag | example | Common Tags | ||||
| Encounter.meta.tag:Source | example | Common Tags | ||||
| Encounter.meta.tag:Provenance | example | Common Tags | ||||
| Encounter.language | extensible | Common Languages
| ||||
| Encounter.identifier.use | required | IdentifierUse | ||||
| Encounter.identifier.type | extensible | Identifier Type Codes | ||||
| Encounter.identifier:localIdentifier.use | required | IdentifierUse | ||||
| Encounter.identifier:localIdentifier.type | extensible | Identifier Type Codes | ||||
| Encounter.status | required | EncounterStatus | ||||
| Encounter.statusHistory.status | required | EncounterStatus | ||||
| Encounter.class | required | InterweaveEncounterClass | ||||
| Encounter.classHistory.class | extensible | ActEncounterCode | ||||
| Encounter.type | required | Care Connect Encounter Type | ||||
| Encounter.type.coding:snomedCT | required | Care Connect Encounter Type | ||||
| Encounter.priority | required | InterweaveEncounterPriority | ||||
| Encounter.participant.type | required | ParticipantType | ||||
| Encounter.reason | preferred | Interweave R4 Encounter Reason | ||||
| Encounter.diagnosis.role | required | DiagnosisRole | ||||
| Encounter.diagnosis:chiefComplaint.role | preferred | Fixed Value: CC("Chief complaint") | ||||
| Encounter.hospitalization.preAdmissionIdentifier.use | required | IdentifierUse | ||||
| Encounter.hospitalization.preAdmissionIdentifier.type | extensible | Identifier Type Codes | ||||
| Encounter.hospitalization.admitSource | required | Interweave Admission Source codes | ||||
| Encounter.hospitalization.reAdmission | example | v2 Re-Admission Indicator | ||||
| Encounter.hospitalization.dietPreference | extensible | Diet | ||||
| Encounter.hospitalization.specialCourtesy | preferred | SpecialCourtesy | ||||
| Encounter.hospitalization.specialArrangement | preferred | SpecialArrangements | ||||
| Encounter.hospitalization.dischargeDisposition | required | Interweave Discharge Destination codes | ||||
| Encounter.location.status | required | EncounterLocationStatus |
Constraints
| Id | Grade | Path(s) | Details | Requirements |
| ele-1 | error | Encounter.extension:encounterTransport, Encounter.extension:outcomeOfAttendance, Encounter.extension:emergencyCareDischargeStatus, Encounter.statusHistory, Encounter.participant, Encounter.diagnosis, Encounter.diagnosis:chiefComplaint, Encounter.hospitalization, Encounter.hospitalization.extension:admissionMethod, Encounter.hospitalization.extension:dischargeMethod, Encounter.location | All FHIR elements must have a @value or children : hasValue() | (children().count() > id.count()) | |
| ext-1 | error | Encounter.extension:encounterTransport, Encounter.extension:outcomeOfAttendance, Encounter.extension:emergencyCareDischargeStatus, Encounter.hospitalization.extension:admissionMethod, Encounter.hospitalization.extension:dischargeMethod | Must have either extensions or value[x], not both : extension.exists() != value.exists() |
This structure is derived from CareConnect-Encounter-1
Summary
Mandatory: 14 elements (43 nested mandatory elements)
Must-Support: 48 elements
Fixed Value: 4 elements
Prohibited: 3 elements
Structures
This structure refers to these other structures:
- CareConnectPatient1 (https://fhir.hl7.org.uk/STU3/StructureDefinition/CareConnect-Patient-1)
- CareConnect-Practitioner-1 (https://fhir.hl7.org.uk/STU3/StructureDefinition/CareConnect-Practitioner-1)
- CareConnect-Condition-1 (https://fhir.hl7.org.uk/STU3/StructureDefinition/CareConnect-Condition-1)
- InterweaveEncounterGrouping (https://fhir.yhcr.nhs.uk/StructureDefinition/Interweave-EncounterGrouping)
Extensions
This structure refers to these extensions:
- https://fhir.yhcr.nhs.uk/StructureDefinition/Extension-Interweave-EDDischargeDestination
- https://fhir.yhcr.nhs.uk/StructureDefinition/Extension-Interweave-R4EncounterServiceType
- https://fhir.yhcr.nhs.uk/StructureDefinition/Extension-Interweave-MedicallySafeForDischarge
Slices
This structure defines the following Slices:
- The element Encounter.meta.tag is sliced based on the value of value:system
- The element Encounter.identifier is sliced based on the value of value:system
- The element Encounter.diagnosis is sliced based on the value of value:role
Differential View
This structure is derived from CareConnect-Encounter-1
| Name | Flags | Card. | Type | Description & Constraints |
|---|---|---|---|---|
 | 0..* | CareConnect-Encounter-1 | An interaction during which services are provided to the patient | |
  | S | 0..1 | id | Logical id of this artifact |
  | ||||
   | S | 0..1 | id | Version specific identifier |
   | S | 0..1 | instant | MANDATORY except in Contained Resources. When the resource version last changed. |
   | S | 0..* | uri | Profiles this resource claims to conform to. Should list (i) this profile (ii) underlying CareConnect profile |
   | 0..* | Coding | DISCOURAGED - may not be honoured by Data Consumers | |
   | 0..* | Coding | Tags applied to this resource Slice: Unordered, Open by value:system | |
    | S | 0..1 | Coding | MANDATORY except in Contained Resources. The Data Provider Id (and display text) of the system supplying the data |
     | 1..1 | uri | Identity of the terminology system Fixed Value: https://yhcr.nhs.uk/Source | |
     | S | 1..1 | code | The Data Provider Id of the system supplying the data |
     | S | 1..1 | string | Name of the system supplying the data |
    | S | 0..1 | Coding | MANDATORY except in Contained Resources. The ODS Code (and display text) of the organisation responsible for the data |
     | 1..1 | uri | Identity of the terminology system Fixed Value: https://yhcr.nhs.uk/Provenance | |
     | S | 1..1 | code | The ODS Code of the organisation responsible for the data |
     | S | 1..1 | string | Name of the organisation supplying the data |
  | 0..1 | uri | DISCOURAGED - may not be honoured by Data Consumers | |
  | 0..1 | code | English is assumed (not currently a multi-lingual implementation) | |
  | 0..1 | Narrative | DISCOURAGED - the preferred approach is to offer structured data fields which a Data Consumer can then render and present in a manner most suited to its users | |
  | S | 0..1 | Extension-CareConnect-OutcomeOfAttendance-1 | An extension to the Encounter resource to record the outcome of an Out-Patient attendance. |
  | S | 0..1 | Extension-CareConnect-EmergencyCareDischargeStatus-1 | An extension to the Encounter resource which is used indicate the status of the Patient on discharge from an Emergency Care Department. |
  | S | 0..1 | CodeableConcept | Discharge destination of patients which have attended ED. URL: https://fhir.yhcr.nhs.uk/StructureDefinition/Extension-Interweave-EDDischargeDestination Binding: Interweave ED Discharge Destination (preferred) |
  | S | 0..1 | CodeableConcept | Specific type of service (pre-adopted from R4) URL: https://fhir.yhcr.nhs.uk/StructureDefinition/Extension-Interweave-R4EncounterServiceType Binding: Interweave UkCore Care Setting Type (preferred) |
  | 0..* | Identifier | Identifier(s) by which this encounter is known Slice: Unordered, Open by value:system | |
   | S | 0..1 | Identifier | Identifier(s) by which this encounter is known |
    | S | 1..1 | uri | The namespace for the identifier value Fixed Value: https://fhir.yhcr.nhs.uk/Id/local-encounter-identifier |
    | S | 1..1 | string | The Local encounter Identifier. Please prefix with ODS code plus period (XXX.) to ensure unique |
    | 0..0 | |||
  | S | 1..1 | code | arrived | triaged | in-progress | onleave | finished | cancelled + (Note: 'planned' is also possible, but normally represented instead as an Appointment) |
  | S | 0..* | BackboneElement | List of past encounter statuses |
  | S | 1..1 | Coding | Classification of the encounter. EXTENSIBLE on request, eg to cover other care settings Binding: InterweaveEncounterClass (required) |
   | 1..1 | uri | Identity of the terminology system | |
   | 1..1 | code | Symbol in syntax defined by the system | |
   | 1..1 | string | Representation defined by the system | |
  | 0..0 | |||
  | S | 0..1 | CodeableConcept | Specific type of encounter Binding: Care Connect Encounter Type (required) |
   | 1..1 | Coding | Code defined by a terminology system | |
    | 1..1 | uri | Identity of the terminology system | |
    | 1..1 | code | Symbol in syntax defined by the system | |
    | 1..1 | string | Representation defined by the system | |
   | S | 1..* | Coding | Code defined by a terminology system Binding: Care Connect Encounter Type (required) |
  | S | 0..1 | CodeableConcept | Indicates the urgency of the encounter Binding: InterweaveEncounterPriority (required) |
   | ||||
    | 1..1 | uri | Identity of the terminology system | |
    | 1..1 | code | Symbol in syntax defined by the system | |
    | 1..1 | string | Representation defined by the system | |
  | S | 1..1 | Reference(CareConnectPatient1) | The patient (NOT group) present at the encounter |
   | 1..1 | string | Reference to a resource (could be Contained) | |
   | 0..1 | Identifier | If relevant could include an id | |
   | 1..1 | string | Description of the referenced resource | |
  | ||||
   | 1..1 | string | Reference to a resource (could be Contained) | |
   | 0..1 | Identifier | If relevant could include an id | |
   | 0..1 | string | If relevant, description of the referenced resource | |
  | S | 1..* | BackboneElement | List of participants involved in the encounter |
   | S | 1..1 | CodeableConcept | Role of participant in encounter Binding: ParticipantType (required) |
    | ||||
     | 1..1 | uri | Identity of the terminology system | |
     | 1..1 | code | Symbol in syntax defined by the system | |
     | 1..1 | string | Representation defined by the system | |
   | S | 1..1 | Reference(CareConnect-Practitioner-1) | Persons involved in the encounter other than the patient |
    | 1..1 | string | Reference to a resource (could be Contained) | |
    | 0..1 | Identifier | If relevant could include an id | |
    | 1..1 | string | Description of the referenced resource | |
  | S | 0..1 | Reference(Appointment) | The appointment that scheduled this encounter |
   | 1..1 | string | Reference to a resource (could be Contained) | |
   | 0..1 | Identifier | If relevant could include an id | |
   | 0..1 | string | If relevant, description of the referenced resource | |
  | S | 1..1 | Period | The start and end time of the encounter |
   | S | 1..1 | dateTime | Starting time with inclusive boundary |
   | S | 0..1 | dateTime | End time with inclusive boundary, if not ongoing |
  | 0..1 | Duration | Quantity of time the encounter lasted (less time absent). Please use minutes. | |
  | S | 0..* | CodeableConcept | Reason the encounter takes place (code) Binding: Interweave R4 Encounter Reason (preferred) |
   | 0..* | Coding | Code defined by a terminology system | |
    | 1..1 | uri | Identity of the terminology system | |
    | 1..1 | code | Symbol in syntax defined by the system | |
    | 1..1 | string | Representation defined by the system | |
  | S | 0..* | BackboneElement | The list of diagnosis relevant to this encounter Slice: Unordered, Open by value:role |
   | Content/Rules for all slices | |||
    | S | 1..1 | Reference(CareConnect-Condition-1) | Reason the encounter takes place (resource) |
     | 1..1 | string | Reference to a resource (could be Contained) | |
     | 0..1 | Identifier | If relevant could include an id | |
     | 0..1 | string | If relevant, description of the referenced resource | |
    | S | 1..1 | CodeableConcept | Role that this diagnosis has within the encounter (e.g. admission, billing, discharge …) Binding: DiagnosisRole (required) |
     | ||||
      | 1..1 | uri | Identity of the terminology system | |
      | 1..1 | code | Symbol in syntax defined by the system | |
      | 1..1 | string | Representation defined by the system | |
    | S | 1..1 | positiveInt | Ranking of the diagnosis (for each role type) |
   | S | 0..1 | BackboneElement | The list of diagnosis relevant to this encounter |
    | 0..1 | CodeableConcept | Role that this diagnosis has within the encounter (e.g. admission, billing, discharge …) Fixed Value: As shown | |
     | 1..1 | Coding | Code defined by a terminology system Fixed Value: (complex) | |
      | 1..1 | uri | Identity of the terminology system Fixed Value: http://hl7.org/fhir/diagnosis-role | |
      | 1..1 | code | Symbol in syntax defined by the system Fixed Value: CC | |
      | 1..1 | string | Representation defined by the system Fixed Value: Chief complaint | |
  | 0..0 | |||
  | S | 0..1 | BackboneElement | Details about the admission to a healthcare service |
   | S | 0..1 | Extension-CareConnect-AdmissionMethod-1 | An extension to the Encounter resource to record how a Patient was admitted to hospital. |
   | S | 0..1 | Extension-CareConnect-DischargeMethod-1 | An extension to the Encounter resource to record the method of discharge from hospital. |
   | S | 0..1 | (Complex) | Medically Safe for Discharge URL: https://fhir.yhcr.nhs.uk/StructureDefinition/Extension-Interweave-MedicallySafeForDischarge |
   | 0..1 | Reference(CareConnect-Location-1) | The location from which the patient came before admission. Useful to provide if possible, in particular to reference a 'site' if transfered from another institution. | |
    | 1..1 | string | Reference to a resource (could be Contained) | |
    | 0..1 | Identifier | If relevant could include an id | |
    | 1..1 | string | Description of the referenced resource | |
   | S | 0..1 | CodeableConcept | From where patient was admitted (physician referral, transfer) Binding: Interweave Admission Source codes (required) |
    | ||||
     | 1..1 | uri | Identity of the terminology system | |
     | 1..1 | code | Symbol in syntax defined by the system | |
     | 1..1 | string | Representation defined by the system | |
   | 0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing | |
   | 0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing | |
   | 0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing | |
   | S | 0..1 | Reference(CareConnect-Location-1) | Location to which the patient is discharged. Important to provide if known to support discharge planning, and/or to reference a 'site' if transfered to another institution. |
    | 1..1 | string | Reference to a resource (could be Contained) | |
    | 0..1 | Identifier | If relevant could include an id | |
    | 1..1 | string | Description of the referenced resource | |
   | S | 0..1 | CodeableConcept | Category or kind of location after discharge Binding: Interweave Discharge Destination codes (required) |
    | ||||
     | 1..1 | uri | Identity of the terminology system | |
     | 1..1 | code | Symbol in syntax defined by the system | |
     | 1..1 | string | Representation defined by the system | |
  | S | 0..* | BackboneElement | Location the encounter takes place (at Ward level) |
   | S | 1..1 | Reference(CareConnect-Location-1) | Location the encounter takes place |
    | 1..1 | string | Reference to a resource (could be Contained) | |
    | 0..1 | Identifier | If relevant could include an id | |
    | 1..1 | string | Description of the referenced resource | |
   | S | 1..1 | code | planned | active | reserved | completed |
   | S | 1..1 | Period | Time period during which the patient was present at the location |
  | 0..1 | Reference(CareConnect-Organization-1) | DISCOURAGED: This is instead covered via the provenance tags | |
  | 0..1 | Reference(InterweaveEncounterGrouping) | Another Encounter this encounter is part of | |
   | 1..1 | string | Reference to a resource (could be Contained) | |
   | 0..1 | Identifier | If relevant could include an id | |
   | 0..1 | string | If relevant, description of the referenced resource | |
 Documentation for this format Documentation for this format | ||||
Terminology Bindings (Differential)
| Path | Conformance | ValueSet |
| Encounter.class | required | InterweaveEncounterClass |
| Encounter.type | required | Care Connect Encounter Type |
| Encounter.type.coding:snomedCT | required | Care Connect Encounter Type |
| Encounter.priority | required | InterweaveEncounterPriority |
| Encounter.participant.type | required | ParticipantType |
| Encounter.reason | preferred | Interweave R4 Encounter Reason |
| Encounter.diagnosis.role | required | DiagnosisRole |
| Encounter.hospitalization.admitSource | required | Interweave Admission Source codes |
| Encounter.hospitalization.dischargeDisposition | required | Interweave Discharge Destination codes |
Key Elements View
| Name | Flags | Card. | Type | Description & Constraints | ||||
|---|---|---|---|---|---|---|---|---|
 | 0..* | CareConnect-Encounter-1 | An interaction during which services are provided to the patient | |||||
  | SΣ | 0..1 | id | Logical id of this artifact | ||||
  | Σ | 0..1 | Meta | Metadata about the resource | ||||
   | SΣ | 0..1 | id | Version specific identifier | ||||
   | SΣ | 0..1 | instant | MANDATORY except in Contained Resources. When the resource version last changed. | ||||
   | SΣ | 0..* | uri | Profiles this resource claims to conform to. Should list (i) this profile (ii) underlying CareConnect profile | ||||
   | Σ | 0..* | Coding | DISCOURAGED - may not be honoured by Data Consumers Binding: All Security Labels (extensible): Security Labels from the Healthcare Privacy and Security Classification System. | ||||
   | Σ | 0..* | Coding | Tags applied to this resource Slice: Unordered, Open by value:system Binding: Common Tags (example): Codes that represent various types of tags, commonly workflow-related; e.g. "Needs review by Dr. Jones" | ||||
    | SΣ | 0..1 | Coding | MANDATORY except in Contained Resources. The Data Provider Id (and display text) of the system supplying the data Binding: Common Tags (example): Codes that represent various types of tags, commonly workflow-related; e.g. "Needs review by Dr. Jones" | ||||
     | Σ | 1..1 | uri | Identity of the terminology system Fixed Value: https://yhcr.nhs.uk/Source | ||||
     | SΣ | 1..1 | code | The Data Provider Id of the system supplying the data | ||||
     | SΣ | 1..1 | string | Name of the system supplying the data | ||||
    | SΣ | 0..1 | Coding | MANDATORY except in Contained Resources. The ODS Code (and display text) of the organisation responsible for the data Binding: Common Tags (example): Codes that represent various types of tags, commonly workflow-related; e.g. "Needs review by Dr. Jones" | ||||
     | Σ | 1..1 | uri | Identity of the terminology system Fixed Value: https://yhcr.nhs.uk/Provenance | ||||
     | SΣ | 1..1 | code | The ODS Code of the organisation responsible for the data | ||||
     | SΣ | 1..1 | string | Name of the organisation supplying the data | ||||
  | ?!Σ | 0..1 | uri | DISCOURAGED - may not be honoured by Data Consumers | ||||
  | 0..1 | code | English is assumed (not currently a multi-lingual implementation) Binding: Common Languages (extensible): A human language.
| |||||
  | 0..1 | Narrative | DISCOURAGED - the preferred approach is to offer structured data fields which a Data Consumer can then render and present in a manner most suited to its users | |||||
  | 0..1 | (Complex) | Encounter transport URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-CareConnect-EncounterTransport-1 | |||||
  | S | 0..1 | CodeableConcept | An extension to the Encounter resource to record the outcome of an Out-Patient attendance. URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-CareConnect-OutcomeOfAttendance-1 Binding: NHS Data Model and Dictionary Outcome Of Attendance (required): This records the outcome of an Out-Patient Attendance Consultant. | ||||
  | S | 0..1 | CodeableConcept | An extension to the Encounter resource which is used indicate the status of the Patient on discharge from an Emergency Care Department. URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-CareConnect-EmergencyCareDischargeStatus-1 Binding: Care Connect Emergency Care Discharge Status (required): The status of the Patient on discharge from an Emergency Care Department. | ||||
  | S | 0..1 | CodeableConcept | Discharge destination of patients which have attended ED. URL: https://fhir.yhcr.nhs.uk/StructureDefinition/Extension-Interweave-EDDischargeDestination Binding: Interweave ED Discharge Destination (preferred) | ||||
  | S | 0..1 | CodeableConcept | Specific type of service (pre-adopted from R4) URL: https://fhir.yhcr.nhs.uk/StructureDefinition/Extension-Interweave-R4EncounterServiceType Binding: Interweave UkCore Care Setting Type (preferred) | ||||
  | ?! | 0..* | Extension | Extensions that cannot be ignored | ||||
  | Σ | 0..* | Identifier | Identifier(s) by which this encounter is known Slice: Unordered, Open by value:system | ||||
   | Content/Rules for all slices | |||||||
    | ?!Σ | 0..1 | code | usual | official | temp | secondary (If known) Binding: IdentifierUse (required): Identifies the purpose for this identifier, if known . | ||||
    | Σ | 1..1 | uri | The namespace for the identifier value Example General: http://www.acme.com/identifiers/patient | ||||
    | Σ | 1..1 | string | The value that is unique Example General: 123456 | ||||
   | SΣ | 0..1 | Identifier | Identifier(s) by which this encounter is known | ||||
    | ?!Σ | 0..1 | code | usual | official | temp | secondary (If known) Binding: IdentifierUse (required): Identifies the purpose for this identifier, if known . | ||||
    | SΣ | 1..1 | uri | The namespace for the identifier value Fixed Value: https://fhir.yhcr.nhs.uk/Id/local-encounter-identifier | ||||
    | SΣ | 1..1 | string | The Local encounter Identifier. Please prefix with ODS code plus period (XXX.) to ensure unique Example General: 123456 | ||||
  | ?!SΣ | 1..1 | code | arrived | triaged | in-progress | onleave | finished | cancelled + (Note: 'planned' is also possible, but normally represented instead as an Appointment) Binding: EncounterStatus (required): Current state of the encounter | ||||
  | S | 0..* | BackboneElement | List of past encounter statuses | ||||
   | ?!Σ | 0..* | Extension | Extensions that cannot be ignored | ||||
   | 1..1 | code | planned | arrived | triaged | in-progress | onleave | finished | cancelled + Binding: EncounterStatus (required): Current state of the encounter | |||||
   | 1..1 | Period | The time that the episode was in the specified status | |||||
  | SΣ | 1..1 | Coding | Classification of the encounter. EXTENSIBLE on request, eg to cover other care settings Binding: InterweaveEncounterClass (required) | ||||
   | Σ | 1..1 | uri | Identity of the terminology system | ||||
   | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
   | Σ | 1..1 | string | Representation defined by the system | ||||
  | SΣ | 0..1 | CodeableConcept | Specific type of encounter Binding: Care Connect Encounter Type (required) | ||||
   | Σ | 1..1 | Coding | Code defined by a terminology system Slice: Unordered, Open by value:system | ||||
    | Content/Rules for all slices | |||||||
     | Σ | 1..1 | uri | Identity of the terminology system | ||||
     | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
     | Σ | 1..1 | string | Representation defined by the system | ||||
    | SΣ | 1..* | Coding | Code defined by a terminology system Binding: Care Connect Encounter Type (required) | ||||
     | 0..* | (Complex) | The SNOMED CT Description ID for the display URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-coding-sctdescid | |||||
     | Σ | 1..1 | uri | Identity of the terminology system Fixed Value: http://snomed.info/sct | ||||
     | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
     | Σ | 1..1 | string | Representation defined by the system | ||||
  | S | 0..1 | CodeableConcept | Indicates the urgency of the encounter Binding: InterweaveEncounterPriority (required) | ||||
  | SΣ | 1..1 | Reference(CareConnectPatient1) | The patient (NOT group) present at the encounter | ||||
   | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
   | Σ | 0..1 | Identifier | If relevant could include an id | ||||
   | Σ | 1..1 | string | Description of the referenced resource | ||||
  | SΣ | 1..* | BackboneElement | List of participants involved in the encounter | ||||
   | ?!Σ | 0..* | Extension | Extensions that cannot be ignored | ||||
   | SΣ | 1..1 | CodeableConcept | Role of participant in encounter Binding: ParticipantType (required) | ||||
   | SΣ | 1..1 | Reference(CareConnect-Practitioner-1) | Persons involved in the encounter other than the patient | ||||
    | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    | Σ | 0..1 | Identifier | If relevant could include an id | ||||
    | Σ | 1..1 | string | Description of the referenced resource | ||||
  | SΣ | 0..1 | Reference(Appointment) | The appointment that scheduled this encounter | ||||
   | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
   | Σ | 0..1 | Identifier | If relevant could include an id | ||||
   | Σ | 0..1 | string | If relevant, description of the referenced resource | ||||
  | S | 1..1 | Period | The start and end time of the encounter | ||||
   | SΣC | 1..1 | dateTime | Starting time with inclusive boundary | ||||
   | SΣC | 0..1 | dateTime | End time with inclusive boundary, if not ongoing | ||||
  | 0..1 | Duration | Quantity of time the encounter lasted (less time absent). Please use minutes. | |||||
  | SΣ | 0..* | CodeableConcept | Reason the encounter takes place (code) Binding: Interweave R4 Encounter Reason (preferred) | ||||
   | Σ | 0..* | Coding | Code defined by a terminology system Slice: Unordered, Open by value:system | ||||
    | Content/Rules for all slices | |||||||
     | Σ | 1..1 | uri | Identity of the terminology system | ||||
     | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
     | Σ | 1..1 | string | Representation defined by the system | ||||
    | Σ | 0..1 | Coding | Code defined by a terminology system | ||||
     | 0..* | (Complex) | The SNOMED CT Description ID for the display URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-coding-sctdescid | |||||
     | Σ | 1..1 | uri | Identity of the terminology system Fixed Value: http://snomed.info/sct | ||||
     | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
     | Σ | 1..1 | string | Representation defined by the system | ||||
  | SΣ | 0..* | BackboneElement | The list of diagnosis relevant to this encounter Slice: Unordered, Open by value:role | ||||
   | Content/Rules for all slices | |||||||
    | ?!Σ | 0..* | Extension | Extensions that cannot be ignored | ||||
    | S | 1..1 | Reference(CareConnect-Condition-1) | Reason the encounter takes place (resource) | ||||
     | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
     | Σ | 0..1 | Identifier | If relevant could include an id | ||||
     | Σ | 0..1 | string | If relevant, description of the referenced resource | ||||
    | S | 1..1 | CodeableConcept | Role that this diagnosis has within the encounter (e.g. admission, billing, discharge …) Binding: DiagnosisRole (required) | ||||
    | S | 1..1 | positiveInt | Ranking of the diagnosis (for each role type) | ||||
   | SΣ | 0..1 | BackboneElement | The list of diagnosis relevant to this encounter | ||||
    | ?!Σ | 0..* | Extension | Extensions that cannot be ignored | ||||
    | 1..1 | Reference(CareConnect-Procedure-1 | CareConnect-Condition-1) | Reason the encounter takes place (resource) | |||||
    | 0..1 | CodeableConcept | Role that this diagnosis has within the encounter (e.g. admission, billing, discharge …) Binding: DiagnosisRole (preferred): The type of diagnosis this condition represents Fixed Value: As shown | |||||
     | 0..0 | string | xml:id (or equivalent in JSON) | |||||
     | 0..0 | Extension | Additional Content defined by implementations | |||||
     | 1..1 | Coding | Code defined by a terminology system Fixed Value: (complex) | |||||
      | 0..0 | string | xml:id (or equivalent in JSON) | |||||
      | 0..0 | Extension | Additional Content defined by implementations | |||||
      | 1..1 | uri | Identity of the terminology system Fixed Value: http://hl7.org/fhir/diagnosis-role | |||||
      | 0..0 | string | Version of the system - if relevant | |||||
      | 1..1 | code | Symbol in syntax defined by the system Fixed Value: CC | |||||
      | 1..1 | string | Representation defined by the system Fixed Value: Chief complaint | |||||
      | 0..0 | boolean | If this coding was chosen directly by the user | |||||
     | 0..0 | string | Plain text representation of the concept | |||||
  | S | 0..1 | BackboneElement | Details about the admission to a healthcare service | ||||
   | S | 0..1 | CodeableConcept | An extension to the Encounter resource to record how a Patient was admitted to hospital. URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-CareConnect-AdmissionMethod-1 Binding: NHS Data Model and Dictionary Admission Method (required): The method of admission to a Hospital Provider Spell. | ||||
   | S | 0..1 | CodeableConcept | An extension to the Encounter resource to record the method of discharge from hospital. URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-CareConnect-DischargeMethod-1 Binding: NHS Data Model and Dictionary Discharge Method (required): The method of discharge from a Hospital Provider Spell. | ||||
   | S | 0..1 | (Complex) | Medically Safe for Discharge URL: https://fhir.yhcr.nhs.uk/StructureDefinition/Extension-Interweave-MedicallySafeForDischarge | ||||
   | ?!Σ | 0..* | Extension | Extensions that cannot be ignored | ||||
   | 0..1 | Reference(CareConnect-Location-1) | The location from which the patient came before admission. Useful to provide if possible, in particular to reference a 'site' if transfered from another institution. | |||||
    | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    | Σ | 0..1 | Identifier | If relevant could include an id | ||||
    | Σ | 1..1 | string | Description of the referenced resource | ||||
   | S | 0..1 | CodeableConcept | From where patient was admitted (physician referral, transfer) Binding: Interweave Admission Source codes (required) | ||||
   | 0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing Binding: Diet (extensible) | |||||
   | 0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing Binding: SpecialCourtesy (preferred): Special courtesies | |||||
   | 0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing Binding: SpecialArrangements (preferred): Special arrangements | |||||
   | S | 0..1 | Reference(CareConnect-Location-1) | Location to which the patient is discharged. Important to provide if known to support discharge planning, and/or to reference a 'site' if transfered to another institution. | ||||
    | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    | Σ | 0..1 | Identifier | If relevant could include an id | ||||
    | Σ | 1..1 | string | Description of the referenced resource | ||||
   | S | 0..1 | CodeableConcept | Category or kind of location after discharge Binding: Interweave Discharge Destination codes (required) | ||||
  | S | 0..* | BackboneElement | Location the encounter takes place (at Ward level) | ||||
   | ?!Σ | 0..* | Extension | Extensions that cannot be ignored | ||||
   | S | 1..1 | Reference(CareConnect-Location-1) | Location the encounter takes place | ||||
    | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    | Σ | 0..1 | Identifier | If relevant could include an id | ||||
    | Σ | 1..1 | string | Description of the referenced resource | ||||
   | S | 1..1 | code | planned | active | reserved | completed Binding: EncounterLocationStatus (required): The status of the location. | ||||
   | S | 1..1 | Period | Time period during which the patient was present at the location | ||||
  | 0..1 | Reference(CareConnect-Organization-1) | DISCOURAGED: This is instead covered via the provenance tags | |||||
  | 0..1 | Reference(InterweaveEncounterGrouping) | Another Encounter this encounter is part of | |||||
   | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
   | Σ | 0..1 | Identifier | If relevant could include an id | ||||
   | Σ | 0..1 | string | If relevant, description of the referenced resource | ||||
 Documentation for this format Documentation for this format | ||||||||
Terminology Bindings
| Path | Conformance | ValueSet / Code | ||||
| Encounter.meta.security | extensible | All Security Labels | ||||
| Encounter.meta.tag | example | Common Tags | ||||
| Encounter.meta.tag:Source | example | Common Tags | ||||
| Encounter.meta.tag:Provenance | example | Common Tags | ||||
| Encounter.language | extensible | Common Languages
| ||||
| Encounter.identifier.use | required | IdentifierUse | ||||
| Encounter.identifier:localIdentifier.use | required | IdentifierUse | ||||
| Encounter.status | required | EncounterStatus | ||||
| Encounter.statusHistory.status | required | EncounterStatus | ||||
| Encounter.class | required | InterweaveEncounterClass | ||||
| Encounter.classHistory.class | extensible | ActEncounterCode | ||||
| Encounter.type | required | Care Connect Encounter Type | ||||
| Encounter.type.coding:snomedCT | required | Care Connect Encounter Type | ||||
| Encounter.priority | required | InterweaveEncounterPriority | ||||
| Encounter.participant.type | required | ParticipantType | ||||
| Encounter.reason | preferred | Interweave R4 Encounter Reason | ||||
| Encounter.diagnosis.role | required | DiagnosisRole | ||||
| Encounter.diagnosis:chiefComplaint.role | preferred | Fixed Value: CC("Chief complaint") | ||||
| Encounter.hospitalization.admitSource | required | Interweave Admission Source codes | ||||
| Encounter.hospitalization.dietPreference | extensible | Diet | ||||
| Encounter.hospitalization.specialCourtesy | preferred | SpecialCourtesy | ||||
| Encounter.hospitalization.specialArrangement | preferred | SpecialArrangements | ||||
| Encounter.hospitalization.dischargeDisposition | required | Interweave Discharge Destination codes | ||||
| Encounter.location.status | required | EncounterLocationStatus |
Constraints
| Id | Grade | Path(s) | Details | Requirements |
| dom-1 | error | Encounter | If the resource is contained in another resource, it SHALL NOT contain any narrative : contained.text.empty() | |
| dom-2 | error | Encounter | If the resource is contained in another resource, it SHALL NOT contain nested Resources : contained.contained.empty() | |
| dom-3 | error | Encounter | If the resource is contained in another resource, it SHALL be referred to from elsewhere in the resource : contained.where(('#'+id in %resource.descendants().reference).not()).empty() | |
| dom-4 | error | Encounter | If a resource is contained in another resource, it SHALL NOT have a meta.versionId or a meta.lastUpdated : contained.meta.versionId.empty() and contained.meta.lastUpdated.empty() | |
| ele-1 | error | Encounter.extension:encounterTransport, Encounter.extension:outcomeOfAttendance, Encounter.extension:emergencyCareDischargeStatus, Encounter.statusHistory, Encounter.participant, Encounter.diagnosis, Encounter.diagnosis:chiefComplaint, Encounter.hospitalization, Encounter.hospitalization.extension:admissionMethod, Encounter.hospitalization.extension:dischargeMethod, Encounter.location | All FHIR elements must have a @value or children : hasValue() | (children().count() > id.count()) | |
| ext-1 | error | Encounter.extension:encounterTransport, Encounter.extension:outcomeOfAttendance, Encounter.extension:emergencyCareDischargeStatus, Encounter.hospitalization.extension:admissionMethod, Encounter.hospitalization.extension:dischargeMethod | Must have either extensions or value[x], not both : extension.exists() != value.exists() |
Snapshot View
| Name | Flags | Card. | Type | Description & Constraints | ||||
|---|---|---|---|---|---|---|---|---|
 | 0..* | CareConnect-Encounter-1 | An interaction during which services are provided to the patient | |||||
  | SΣ | 0..1 | id | Logical id of this artifact | ||||
  | Σ | 0..1 | Meta | Metadata about the resource | ||||
   | 0..1 | string | xml:id (or equivalent in JSON) | |||||
   | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
   | SΣ | 0..1 | id | Version specific identifier | ||||
   | SΣ | 0..1 | instant | MANDATORY except in Contained Resources. When the resource version last changed. | ||||
   | SΣ | 0..* | uri | Profiles this resource claims to conform to. Should list (i) this profile (ii) underlying CareConnect profile | ||||
   | Σ | 0..* | Coding | DISCOURAGED - may not be honoured by Data Consumers Binding: All Security Labels (extensible): Security Labels from the Healthcare Privacy and Security Classification System. | ||||
   | Σ | 0..* | Coding | Tags applied to this resource Slice: Unordered, Open by value:system Binding: Common Tags (example): Codes that represent various types of tags, commonly workflow-related; e.g. "Needs review by Dr. Jones" | ||||
    | SΣ | 0..1 | Coding | MANDATORY except in Contained Resources. The Data Provider Id (and display text) of the system supplying the data Binding: Common Tags (example): Codes that represent various types of tags, commonly workflow-related; e.g. "Needs review by Dr. Jones" | ||||
     | 0..1 | string | xml:id (or equivalent in JSON) | |||||
     | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
     | Σ | 1..1 | uri | Identity of the terminology system Fixed Value: https://yhcr.nhs.uk/Source | ||||
     | Σ | 0..1 | string | Version of the system - if relevant | ||||
     | SΣ | 1..1 | code | The Data Provider Id of the system supplying the data | ||||
     | SΣ | 1..1 | string | Name of the system supplying the data | ||||
     | Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
    | SΣ | 0..1 | Coding | MANDATORY except in Contained Resources. The ODS Code (and display text) of the organisation responsible for the data Binding: Common Tags (example): Codes that represent various types of tags, commonly workflow-related; e.g. "Needs review by Dr. Jones" | ||||
     | 0..1 | string | xml:id (or equivalent in JSON) | |||||
     | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
     | Σ | 1..1 | uri | Identity of the terminology system Fixed Value: https://yhcr.nhs.uk/Provenance | ||||
     | Σ | 0..1 | string | Version of the system - if relevant | ||||
     | SΣ | 1..1 | code | The ODS Code of the organisation responsible for the data | ||||
     | SΣ | 1..1 | string | Name of the organisation supplying the data | ||||
     | Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
  | ?!Σ | 0..1 | uri | DISCOURAGED - may not be honoured by Data Consumers | ||||
  | 0..1 | code | English is assumed (not currently a multi-lingual implementation) Binding: Common Languages (extensible): A human language.
| |||||
  | 0..1 | Narrative | DISCOURAGED - the preferred approach is to offer structured data fields which a Data Consumer can then render and present in a manner most suited to its users | |||||
  | 0..* | Resource | Contained, inline Resources | |||||
  | 0..* | Extension | Extension Slice: Unordered, Open by value:url | |||||
  | 0..1 | (Complex) | Encounter transport URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-CareConnect-EncounterTransport-1 | |||||
  | S | 0..1 | CodeableConcept | An extension to the Encounter resource to record the outcome of an Out-Patient attendance. URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-CareConnect-OutcomeOfAttendance-1 Binding: NHS Data Model and Dictionary Outcome Of Attendance (required): This records the outcome of an Out-Patient Attendance Consultant. | ||||
  | S | 0..1 | CodeableConcept | An extension to the Encounter resource which is used indicate the status of the Patient on discharge from an Emergency Care Department. URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-CareConnect-EmergencyCareDischargeStatus-1 Binding: Care Connect Emergency Care Discharge Status (required): The status of the Patient on discharge from an Emergency Care Department. | ||||
  | S | 0..1 | CodeableConcept | Discharge destination of patients which have attended ED. URL: https://fhir.yhcr.nhs.uk/StructureDefinition/Extension-Interweave-EDDischargeDestination Binding: Interweave ED Discharge Destination (preferred) | ||||
  | S | 0..1 | CodeableConcept | Specific type of service (pre-adopted from R4) URL: https://fhir.yhcr.nhs.uk/StructureDefinition/Extension-Interweave-R4EncounterServiceType Binding: Interweave UkCore Care Setting Type (preferred) | ||||
  | ?! | 0..* | Extension | Extensions that cannot be ignored | ||||
  | Σ | 0..* | Identifier | Identifier(s) by which this encounter is known Slice: Unordered, Open by value:system | ||||
   | Content/Rules for all slices | |||||||
    | 0..1 | string | xml:id (or equivalent in JSON) | |||||
    | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
    | ?!Σ | 0..1 | code | usual | official | temp | secondary (If known) Binding: IdentifierUse (required): Identifies the purpose for this identifier, if known . | ||||
    | Σ | 0..1 | CodeableConcept | Description of identifier Binding: Identifier Type Codes (extensible): A coded type for an identifier that can be used to determine which identifier to use for a specific purpose. | ||||
    | Σ | 1..1 | uri | The namespace for the identifier value Example General: http://www.acme.com/identifiers/patient | ||||
    | Σ | 1..1 | string | The value that is unique Example General: 123456 | ||||
    | Σ | 0..1 | Period | Time period when id is/was valid for use | ||||
    | Σ | 0..1 | Reference(CareConnect-Organization-1) | Organization that issued id (may be just text) | ||||
   | SΣ | 0..1 | Identifier | Identifier(s) by which this encounter is known | ||||
    | 0..1 | string | xml:id (or equivalent in JSON) | |||||
    | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
    | ?!Σ | 0..1 | code | usual | official | temp | secondary (If known) Binding: IdentifierUse (required): Identifies the purpose for this identifier, if known . | ||||
    | Σ | 0..1 | CodeableConcept | Description of identifier Binding: Identifier Type Codes (extensible): A coded type for an identifier that can be used to determine which identifier to use for a specific purpose. | ||||
    | SΣ | 1..1 | uri | The namespace for the identifier value Fixed Value: https://fhir.yhcr.nhs.uk/Id/local-encounter-identifier | ||||
    | SΣ | 1..1 | string | The Local encounter Identifier. Please prefix with ODS code plus period (XXX.) to ensure unique Example General: 123456 | ||||
    | Σ | 0..1 | Reference(CareConnect-Organization-1) | Organization that issued id (may be just text) | ||||
  | ?!SΣ | 1..1 | code | arrived | triaged | in-progress | onleave | finished | cancelled + (Note: 'planned' is also possible, but normally represented instead as an Appointment) Binding: EncounterStatus (required): Current state of the encounter | ||||
  | S | 0..* | BackboneElement | List of past encounter statuses | ||||
   | 0..1 | string | xml:id (or equivalent in JSON) | |||||
   | 0..* | Extension | Additional Content defined by implementations | |||||
   | ?!Σ | 0..* | Extension | Extensions that cannot be ignored | ||||
   | 1..1 | code | planned | arrived | triaged | in-progress | onleave | finished | cancelled + Binding: EncounterStatus (required): Current state of the encounter | |||||
   | 1..1 | Period | The time that the episode was in the specified status | |||||
  | SΣ | 1..1 | Coding | Classification of the encounter. EXTENSIBLE on request, eg to cover other care settings Binding: InterweaveEncounterClass (required) | ||||
   | 0..1 | string | xml:id (or equivalent in JSON) | |||||
   | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
   | Σ | 1..1 | uri | Identity of the terminology system | ||||
   | Σ | 0..1 | string | Version of the system - if relevant | ||||
   | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
   | Σ | 1..1 | string | Representation defined by the system | ||||
   | Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
  | SΣ | 0..1 | CodeableConcept | Specific type of encounter Binding: Care Connect Encounter Type (required) | ||||
   | 0..1 | string | xml:id (or equivalent in JSON) | |||||
   | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
   | Σ | 1..1 | Coding | Code defined by a terminology system Slice: Unordered, Open by value:system | ||||
    | Content/Rules for all slices | |||||||
     | 0..1 | string | xml:id (or equivalent in JSON) | |||||
     | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
     | Σ | 1..1 | uri | Identity of the terminology system | ||||
     | Σ | 0..1 | string | Version of the system - if relevant | ||||
     | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
     | Σ | 1..1 | string | Representation defined by the system | ||||
     | Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
    | SΣ | 1..* | Coding | Code defined by a terminology system Binding: Care Connect Encounter Type (required) | ||||
     | 0..1 | string | xml:id (or equivalent in JSON) | |||||
     | 0..* | Extension | Extension Slice: Unordered, Open by value:url | |||||
     | 0..* | (Complex) | The SNOMED CT Description ID for the display URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-coding-sctdescid | |||||
     | Σ | 1..1 | uri | Identity of the terminology system Fixed Value: http://snomed.info/sct | ||||
     | Σ | 0..1 | string | Version of the system - if relevant | ||||
     | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
     | Σ | 1..1 | string | Representation defined by the system | ||||
     | Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
   | Σ | 0..1 | string | Plain text representation of the concept | ||||
  | S | 0..1 | CodeableConcept | Indicates the urgency of the encounter Binding: InterweaveEncounterPriority (required) | ||||
   | 0..1 | string | xml:id (or equivalent in JSON) | |||||
   | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
   | Σ | 0..* | Coding | Code defined by a terminology system | ||||
    | 0..1 | string | xml:id (or equivalent in JSON) | |||||
    | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
    | Σ | 1..1 | uri | Identity of the terminology system | ||||
    | Σ | 0..1 | string | Version of the system - if relevant | ||||
    | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
    | Σ | 1..1 | string | Representation defined by the system | ||||
    | Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
   | Σ | 0..1 | string | Plain text representation of the concept | ||||
  | SΣ | 1..1 | Reference(CareConnectPatient1) | The patient (NOT group) present at the encounter | ||||
   | 0..1 | string | xml:id (or equivalent in JSON) | |||||
   | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
   | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
   | Σ | 0..1 | Identifier | If relevant could include an id | ||||
   | Σ | 1..1 | string | Description of the referenced resource | ||||
  | Σ | 0..* | Reference(EpisodeOfCare) | Episode(s) of care that this encounter should be recorded against | ||||
  | 0..* | Reference(ReferralRequest) | The ReferralRequest that initiated this encounter | |||||
   | 0..1 | string | xml:id (or equivalent in JSON) | |||||
   | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
   | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
   | Σ | 0..1 | Identifier | If relevant could include an id | ||||
   | Σ | 0..1 | string | If relevant, description of the referenced resource | ||||
  | SΣ | 1..* | BackboneElement | List of participants involved in the encounter | ||||
   | 0..1 | string | xml:id (or equivalent in JSON) | |||||
   | 0..* | Extension | Additional Content defined by implementations | |||||
   | ?!Σ | 0..* | Extension | Extensions that cannot be ignored | ||||
   | SΣ | 1..1 | CodeableConcept | Role of participant in encounter Binding: ParticipantType (required) | ||||
    | 0..1 | string | xml:id (or equivalent in JSON) | |||||
    | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
    | Σ | 0..* | Coding | Code defined by a terminology system | ||||
     | 0..1 | string | xml:id (or equivalent in JSON) | |||||
     | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
     | Σ | 1..1 | uri | Identity of the terminology system | ||||
     | Σ | 0..1 | string | Version of the system - if relevant | ||||
     | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
     | Σ | 1..1 | string | Representation defined by the system | ||||
     | Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
    | Σ | 0..1 | string | Plain text representation of the concept | ||||
   | 0..1 | Period | Period of time during the encounter that the participant participated | |||||
   | SΣ | 1..1 | Reference(CareConnect-Practitioner-1) | Persons involved in the encounter other than the patient | ||||
    | 0..1 | string | xml:id (or equivalent in JSON) | |||||
    | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
    | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    | Σ | 0..1 | Identifier | If relevant could include an id | ||||
    | Σ | 1..1 | string | Description of the referenced resource | ||||
  | SΣ | 0..1 | Reference(Appointment) | The appointment that scheduled this encounter | ||||
   | 0..1 | string | xml:id (or equivalent in JSON) | |||||
   | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
   | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
   | Σ | 0..1 | Identifier | If relevant could include an id | ||||
   | Σ | 0..1 | string | If relevant, description of the referenced resource | ||||
  | S | 1..1 | Period | The start and end time of the encounter | ||||
   | 0..1 | string | xml:id (or equivalent in JSON) | |||||
   | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
   | SΣC | 1..1 | dateTime | Starting time with inclusive boundary | ||||
   | SΣC | 0..1 | dateTime | End time with inclusive boundary, if not ongoing | ||||
  | 0..1 | Duration | Quantity of time the encounter lasted (less time absent). Please use minutes. | |||||
  | SΣ | 0..* | CodeableConcept | Reason the encounter takes place (code) Binding: Interweave R4 Encounter Reason (preferred) | ||||
   | 0..1 | string | xml:id (or equivalent in JSON) | |||||
   | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
   | Σ | 0..* | Coding | Code defined by a terminology system Slice: Unordered, Open by value:system | ||||
    | Content/Rules for all slices | |||||||
     | 0..1 | string | xml:id (or equivalent in JSON) | |||||
     | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
     | Σ | 1..1 | uri | Identity of the terminology system | ||||
     | Σ | 0..1 | string | Version of the system - if relevant | ||||
     | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
     | Σ | 1..1 | string | Representation defined by the system | ||||
     | Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
    | Σ | 0..1 | Coding | Code defined by a terminology system | ||||
     | 0..1 | string | xml:id (or equivalent in JSON) | |||||
     | 0..* | Extension | Extension Slice: Unordered, Open by value:url | |||||
     | 0..* | (Complex) | The SNOMED CT Description ID for the display URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-coding-sctdescid | |||||
     | Σ | 1..1 | uri | Identity of the terminology system Fixed Value: http://snomed.info/sct | ||||
     | Σ | 0..1 | string | Version of the system - if relevant | ||||
     | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
     | Σ | 1..1 | string | Representation defined by the system | ||||
     | Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
   | Σ | 0..1 | string | Plain text representation of the concept | ||||
  | SΣ | 0..* | BackboneElement | The list of diagnosis relevant to this encounter Slice: Unordered, Open by value:role | ||||
   | Content/Rules for all slices | |||||||
    | 0..1 | string | xml:id (or equivalent in JSON) | |||||
    | 0..* | Extension | Additional Content defined by implementations | |||||
    | ?!Σ | 0..* | Extension | Extensions that cannot be ignored | ||||
    | S | 1..1 | Reference(CareConnect-Condition-1) | Reason the encounter takes place (resource) | ||||
     | 0..1 | string | xml:id (or equivalent in JSON) | |||||
     | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
     | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
     | Σ | 0..1 | Identifier | If relevant could include an id | ||||
     | Σ | 0..1 | string | If relevant, description of the referenced resource | ||||
    | S | 1..1 | CodeableConcept | Role that this diagnosis has within the encounter (e.g. admission, billing, discharge …) Binding: DiagnosisRole (required) | ||||
     | 0..1 | string | xml:id (or equivalent in JSON) | |||||
     | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
     | Σ | 0..* | Coding | Code defined by a terminology system | ||||
      | 0..1 | string | xml:id (or equivalent in JSON) | |||||
      | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
      | Σ | 1..1 | uri | Identity of the terminology system | ||||
      | Σ | 0..1 | string | Version of the system - if relevant | ||||
      | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
      | Σ | 1..1 | string | Representation defined by the system | ||||
      | Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
     | Σ | 0..1 | string | Plain text representation of the concept | ||||
    | S | 1..1 | positiveInt | Ranking of the diagnosis (for each role type) | ||||
   | SΣ | 0..1 | BackboneElement | The list of diagnosis relevant to this encounter | ||||
    | 0..1 | string | xml:id (or equivalent in JSON) | |||||
    | 0..* | Extension | Additional Content defined by implementations | |||||
    | ?!Σ | 0..* | Extension | Extensions that cannot be ignored | ||||
    | 1..1 | Reference(CareConnect-Procedure-1 | CareConnect-Condition-1) | Reason the encounter takes place (resource) | |||||
    | 0..1 | CodeableConcept | Role that this diagnosis has within the encounter (e.g. admission, billing, discharge …) Binding: DiagnosisRole (preferred): The type of diagnosis this condition represents Fixed Value: As shown | |||||
     | 0..0 | string | xml:id (or equivalent in JSON) | |||||
     | 0..0 | Extension | Additional Content defined by implementations | |||||
     | 1..1 | Coding | Code defined by a terminology system Fixed Value: (complex) | |||||
      | 0..0 | string | xml:id (or equivalent in JSON) | |||||
      | 0..0 | Extension | Additional Content defined by implementations | |||||
      | 1..1 | uri | Identity of the terminology system Fixed Value: http://hl7.org/fhir/diagnosis-role | |||||
      | 0..0 | string | Version of the system - if relevant | |||||
      | 1..1 | code | Symbol in syntax defined by the system Fixed Value: CC | |||||
      | 1..1 | string | Representation defined by the system Fixed Value: Chief complaint | |||||
      | 0..0 | boolean | If this coding was chosen directly by the user | |||||
     | 0..0 | string | Plain text representation of the concept | |||||
    | 0..1 | positiveInt | Ranking of the diagnosis (for each role type) | |||||
  | S | 0..1 | BackboneElement | Details about the admission to a healthcare service | ||||
   | 0..1 | string | xml:id (or equivalent in JSON) | |||||
   | 0..* | Extension | Extension Slice: Unordered, Open by value:url | |||||
   | S | 0..1 | CodeableConcept | An extension to the Encounter resource to record how a Patient was admitted to hospital. URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-CareConnect-AdmissionMethod-1 Binding: NHS Data Model and Dictionary Admission Method (required): The method of admission to a Hospital Provider Spell. | ||||
   | S | 0..1 | CodeableConcept | An extension to the Encounter resource to record the method of discharge from hospital. URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-CareConnect-DischargeMethod-1 Binding: NHS Data Model and Dictionary Discharge Method (required): The method of discharge from a Hospital Provider Spell. | ||||
   | S | 0..1 | (Complex) | Medically Safe for Discharge URL: https://fhir.yhcr.nhs.uk/StructureDefinition/Extension-Interweave-MedicallySafeForDischarge | ||||
   | ?!Σ | 0..* | Extension | Extensions that cannot be ignored | ||||
   | 0..1 | Identifier | Pre-admission identifier | |||||
    | 0..1 | string | xml:id (or equivalent in JSON) | |||||
    | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
    | ?!Σ | 0..1 | code | usual | official | temp | secondary (If known) Binding: IdentifierUse (required): Identifies the purpose for this identifier, if known . | ||||
    | Σ | 0..1 | CodeableConcept | Description of identifier Binding: Identifier Type Codes (extensible): A coded type for an identifier that can be used to determine which identifier to use for a specific purpose. | ||||
    | Σ | 1..1 | uri | The namespace for the identifier value Example General: http://www.acme.com/identifiers/patient | ||||
    | Σ | 1..1 | string | The value that is unique Example General: 123456 | ||||
    | Σ | 0..1 | Period | Time period when id is/was valid for use | ||||
    | Σ | 0..1 | Reference(CareConnect-Organization-1) | Organization that issued id (may be just text) | ||||
   | 0..1 | Reference(CareConnect-Location-1) | The location from which the patient came before admission. Useful to provide if possible, in particular to reference a 'site' if transfered from another institution. | |||||
    | 0..1 | string | xml:id (or equivalent in JSON) | |||||
    | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
    | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    | Σ | 0..1 | Identifier | If relevant could include an id | ||||
    | Σ | 1..1 | string | Description of the referenced resource | ||||
   | S | 0..1 | CodeableConcept | From where patient was admitted (physician referral, transfer) Binding: Interweave Admission Source codes (required) | ||||
    | 0..1 | string | xml:id (or equivalent in JSON) | |||||
    | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
    | Σ | 0..* | Coding | Code defined by a terminology system | ||||
     | 0..1 | string | xml:id (or equivalent in JSON) | |||||
     | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
     | Σ | 1..1 | uri | Identity of the terminology system | ||||
     | Σ | 0..1 | string | Version of the system - if relevant | ||||
     | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
     | Σ | 1..1 | string | Representation defined by the system | ||||
     | Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
    | Σ | 0..1 | string | Plain text representation of the concept | ||||
   | 0..1 | CodeableConcept | The type of hospital re-admission that has occurred (if any). If the value is absent, then this is not identified as a readmission Binding: v2 Re-Admission Indicator (example): The reason for re-admission of this hospitalization encounter. | |||||
    | 0..1 | string | xml:id (or equivalent in JSON) | |||||
    | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
    | Σ | 0..* | Coding | Code defined by a terminology system Slice: Unordered, Open by value:system | ||||
     | Σ | 0..1 | Coding | Code defined by a terminology system | ||||
      | 0..1 | string | xml:id (or equivalent in JSON) | |||||
      | 0..* | Extension | Extension Slice: Unordered, Open by value:url | |||||
      | 0..* | (Complex) | The SNOMED CT Description ID for the display URL: https://fhir.hl7.org.uk/STU3/StructureDefinition/Extension-coding-sctdescid | |||||
      | Σ | 1..1 | uri | Identity of the terminology system Fixed Value: http://snomed.info/sct | ||||
      | Σ | 0..1 | string | Version of the system - if relevant | ||||
      | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
      | Σ | 1..1 | string | Representation defined by the system | ||||
      | Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
    | Σ | 0..1 | string | Plain text representation of the concept | ||||
   | 0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing Binding: Diet (extensible) | |||||
   | 0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing Binding: SpecialCourtesy (preferred): Special courtesies | |||||
   | 0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing Binding: SpecialArrangements (preferred): Special arrangements | |||||
   | S | 0..1 | Reference(CareConnect-Location-1) | Location to which the patient is discharged. Important to provide if known to support discharge planning, and/or to reference a 'site' if transfered to another institution. | ||||
    | 0..1 | string | xml:id (or equivalent in JSON) | |||||
    | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
    | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    | Σ | 0..1 | Identifier | If relevant could include an id | ||||
    | Σ | 1..1 | string | Description of the referenced resource | ||||
   | S | 0..1 | CodeableConcept | Category or kind of location after discharge Binding: Interweave Discharge Destination codes (required) | ||||
    | 0..1 | string | xml:id (or equivalent in JSON) | |||||
    | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
    | Σ | 0..* | Coding | Code defined by a terminology system | ||||
     | 0..1 | string | xml:id (or equivalent in JSON) | |||||
     | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
     | Σ | 1..1 | uri | Identity of the terminology system | ||||
     | Σ | 0..1 | string | Version of the system - if relevant | ||||
     | Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
     | Σ | 1..1 | string | Representation defined by the system | ||||
     | Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
    | Σ | 0..1 | string | Plain text representation of the concept | ||||
  | S | 0..* | BackboneElement | Location the encounter takes place (at Ward level) | ||||
   | 0..1 | string | xml:id (or equivalent in JSON) | |||||
   | 0..* | Extension | Additional Content defined by implementations | |||||
   | ?!Σ | 0..* | Extension | Extensions that cannot be ignored | ||||
   | S | 1..1 | Reference(CareConnect-Location-1) | Location the encounter takes place | ||||
    | 0..1 | string | xml:id (or equivalent in JSON) | |||||
    | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
    | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    | Σ | 0..1 | Identifier | If relevant could include an id | ||||
    | Σ | 1..1 | string | Description of the referenced resource | ||||
   | S | 1..1 | code | planned | active | reserved | completed Binding: EncounterLocationStatus (required): The status of the location. | ||||
   | S | 1..1 | Period | Time period during which the patient was present at the location | ||||
  | 0..1 | Reference(CareConnect-Organization-1) | DISCOURAGED: This is instead covered via the provenance tags | |||||
  | 0..1 | Reference(InterweaveEncounterGrouping) | Another Encounter this encounter is part of | |||||
   | 0..1 | string | xml:id (or equivalent in JSON) | |||||
   | 0..* | Extension | Additional Content defined by implementations Slice: Unordered, Open by value:url | |||||
   | ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
   | Σ | 0..1 | Identifier | If relevant could include an id | ||||
   | Σ | 0..1 | string | If relevant, description of the referenced resource | ||||
 Documentation for this format Documentation for this format | ||||||||
Terminology Bindings
| Path | Conformance | ValueSet / Code | ||||
| Encounter.meta.security | extensible | All Security Labels | ||||
| Encounter.meta.tag | example | Common Tags | ||||
| Encounter.meta.tag:Source | example | Common Tags | ||||
| Encounter.meta.tag:Provenance | example | Common Tags | ||||
| Encounter.language | extensible | Common Languages
| ||||
| Encounter.identifier.use | required | IdentifierUse | ||||
| Encounter.identifier.type | extensible | Identifier Type Codes | ||||
| Encounter.identifier:localIdentifier.use | required | IdentifierUse | ||||
| Encounter.identifier:localIdentifier.type | extensible | Identifier Type Codes | ||||
| Encounter.status | required | EncounterStatus | ||||
| Encounter.statusHistory.status | required | EncounterStatus | ||||
| Encounter.class | required | InterweaveEncounterClass | ||||
| Encounter.classHistory.class | extensible | ActEncounterCode | ||||
| Encounter.type | required | Care Connect Encounter Type | ||||
| Encounter.type.coding:snomedCT | required | Care Connect Encounter Type | ||||
| Encounter.priority | required | InterweaveEncounterPriority | ||||
| Encounter.participant.type | required | ParticipantType | ||||
| Encounter.reason | preferred | Interweave R4 Encounter Reason | ||||
| Encounter.diagnosis.role | required | DiagnosisRole | ||||
| Encounter.diagnosis:chiefComplaint.role | preferred | Fixed Value: CC("Chief complaint") | ||||
| Encounter.hospitalization.preAdmissionIdentifier.use | required | IdentifierUse | ||||
| Encounter.hospitalization.preAdmissionIdentifier.type | extensible | Identifier Type Codes | ||||
| Encounter.hospitalization.admitSource | required | Interweave Admission Source codes | ||||
| Encounter.hospitalization.reAdmission | example | v2 Re-Admission Indicator | ||||
| Encounter.hospitalization.dietPreference | extensible | Diet | ||||
| Encounter.hospitalization.specialCourtesy | preferred | SpecialCourtesy | ||||
| Encounter.hospitalization.specialArrangement | preferred | SpecialArrangements | ||||
| Encounter.hospitalization.dischargeDisposition | required | Interweave Discharge Destination codes | ||||
| Encounter.location.status | required | EncounterLocationStatus |
Constraints
| Id | Grade | Path(s) | Details | Requirements |
| ele-1 | error | Encounter.extension:encounterTransport, Encounter.extension:outcomeOfAttendance, Encounter.extension:emergencyCareDischargeStatus, Encounter.statusHistory, Encounter.participant, Encounter.diagnosis, Encounter.diagnosis:chiefComplaint, Encounter.hospitalization, Encounter.hospitalization.extension:admissionMethod, Encounter.hospitalization.extension:dischargeMethod, Encounter.location | All FHIR elements must have a @value or children : hasValue() | (children().count() > id.count()) | |
| ext-1 | error | Encounter.extension:encounterTransport, Encounter.extension:outcomeOfAttendance, Encounter.extension:emergencyCareDischargeStatus, Encounter.hospitalization.extension:admissionMethod, Encounter.hospitalization.extension:dischargeMethod | Must have either extensions or value[x], not both : extension.exists() != value.exists() |
This structure is derived from CareConnect-Encounter-1
Summary
Mandatory: 14 elements (43 nested mandatory elements)
Must-Support: 48 elements
Fixed Value: 4 elements
Prohibited: 3 elements
Structures
This structure refers to these other structures:
- CareConnectPatient1 (https://fhir.hl7.org.uk/STU3/StructureDefinition/CareConnect-Patient-1)
- CareConnect-Practitioner-1 (https://fhir.hl7.org.uk/STU3/StructureDefinition/CareConnect-Practitioner-1)
- CareConnect-Condition-1 (https://fhir.hl7.org.uk/STU3/StructureDefinition/CareConnect-Condition-1)
- InterweaveEncounterGrouping (https://fhir.yhcr.nhs.uk/StructureDefinition/Interweave-EncounterGrouping)
Extensions
This structure refers to these extensions:
- https://fhir.yhcr.nhs.uk/StructureDefinition/Extension-Interweave-EDDischargeDestination
- https://fhir.yhcr.nhs.uk/StructureDefinition/Extension-Interweave-R4EncounterServiceType
- https://fhir.yhcr.nhs.uk/StructureDefinition/Extension-Interweave-MedicallySafeForDischarge
Slices
This structure defines the following Slices:
- The element Encounter.meta.tag is sliced based on the value of value:system
- The element Encounter.identifier is sliced based on the value of value:system
- The element Encounter.diagnosis is sliced based on the value of value:role
Other representations of profile: CSV, Excel, Schematron