Interweave Implementation Guide
0.1.0 - ci-build
Interweave Implementation Guide
0.1.0 - ci-build
Interweave Implementation Guide - Local Development build (v0.1.0) built by the FHIR (HL7® FHIR® Standard) Build Tools. See the STU3 profiles here.
| Official URL: https://fhir.interweavedigital.nhs.uk/R4/StructureDefinition/Interweave-Encounter | Version: 0.0.1 | |||
| Draft as of 2024-07-15 | Computable Name: InterweaveEncounter | |||
Interweave Encounter resource profile - DRAFT.
Status: DRAFT: For Review
This profile sets out the expectations for the interweave Encounter resource. We use the UKCore-Encounter structure definition as a base to this profile.
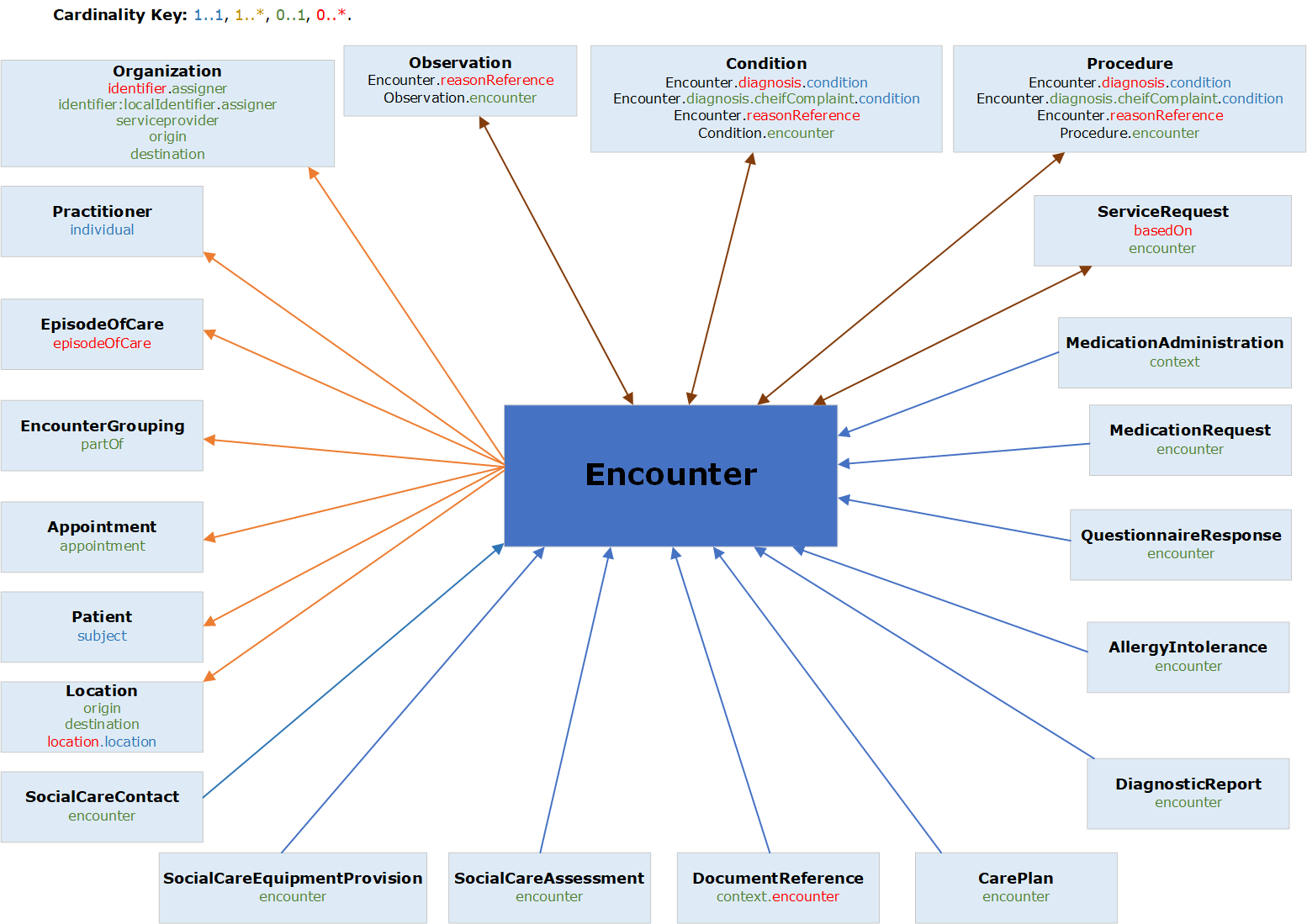
The Encounter is a key resource - as it explains the who, where, when, and why of care that has been provided. Not only is the Encounter resource valuable in itself, but it also acts as a point of reference for linking to other clinical resources.
Its main use in our region at present is for acute care, where it can be used to describe inpatient, outpatient and emergency encounters.
As of this writing Encounters are not being used by Social Care - which instead uses a model based around the Episode of Care. See the Episode of Care profile for further details.
The Encounter is a complex FHIR Resource – and one which offers significant flexibility to support different representations. The FHIR guidance on anticipated usage is helpful and should be read as background, see https://hl7.org/fhir/R4/encounter.html. As this states: “The expectation is that for each domain of exchange, profiles are used to limit the flexibility of Encounter to meet the demands of the use case”. Before looking at the data items in detail, it is therefore necessary to establish some overall guidelines on how the Encounter resource type will be used
Whilst there is an intuitive understanding of what constitutes the start / end of an Encounter, it is challenging to establish a rigorous definition. Nevertheless, the following guidelines cover key points discussed to date:
An Encounter covers a period of continuous care
A change in care-setting constitutes a change of Encounter. (This would include moving from Emergency to Inpatient to Outpatient within a hospital – as indicated by the “class”)
A change in location within the same care setting does NOT constitute a change of Encounter. (For example moving between beds and/or wards within a hospital inpatient stay. This would instead be modelled using the “location” sub-structure of the Encounter)
Involvement of additional clinicians does NOT constitute a separate Encounter. For example, suppose a hospital inpatient is visited by a dietician during their stay:
Any discussion of Encounters inevitably has to consider the topic of how Encounters are structured and grouped.
There is a need to balance the desire to accurately model the complexity of real-life vs the need to provide a simple model which is easy for Data Consumers to understand and to reliably display. Experience suggests that offering a plethora of varying complex hierarchical structures from different care settings makes the task of a Data Consumer extremely challenging.
The core of the approach is therefore a simple flat list of Encounters. Two options are then offered to enrich this with different types of groupings:
Core Model - Simple flat list of Encounters
This is the basic model which all Data Providers and Consumers MUST support. It consists of a simple flat list of Encounters with no hierarchy whatsoever.
The basic model is therefore of standalone Encounters which have a full set of information populated to give a complete picture of what occurred.
A specific implication of this is in the use of the "hospitalization" structure which, despite the name, can be used to convey important admission and discharge information relevant to any care-setting:
Grouping Option 1 - Encounter Grouping (linking in time)
Despite the appeal of a simple flat list of Encounters, the concept of a "visit", "hospitalisation", or "incident" is widely recognised and agreed to be useful as a way of grouping Encounters that are linked in time. For example:
A two-level hierarchy is therefore defined, based on the use of special type of Grouping Encounter to link together Encounters which comprise part of the same "visit", "stay" or "incident".
In practical terms:
Grouping Option 2 - Episode of Care (linking by condition)
Another way of grouping Encounters goes beyond modelling a single visit or incident and links together a care pathway based on a Condition. This linkage is provided by the Episode of Care.
At first glance it can be difficult to distinguish an Encounter Grouping from an Episode of Care - however the FHIR specification provides helpful guidance, and in fact there are some clear differentiating features:
An Episode of Care is based around a "condition" and is thus used to join-up a care pathway. Specifically, a patient with multiple conditions could have multiple Episodes of Care running concurrently. The Episode of Care is used to "pick out" from the mass of activity those Encounters relating to a particular care pathway. Therefore the Episode of Care MUST have its Condition field populated when using it to group Encounters in this way.
Longer term the definition of "organisation" might be considered a point of controversy, specifically is an Integrated Care System an "organisation"? This would provide a valuable mechanism to link up a cross-care-setting care pathway - noting that there is currently no obvious mechanism to identify and link encounters at this whole-system level. Extending an Episode of Care across multiple care settings in this way is therefore currently seen as aspiriational and unlikely to be implemented immediately. Please get in touch for further discussion if you believe you may be a first-of-type.
The diagram below summarises the above discussion - ie core Encounters, plus options for a single Grouping Encounter, and/or one or more Episodes of Care.
Whilst the terms "Encounter" and "Appointment" might be used interchangeably in everyday speech, in FHIR they have specific meanings:
In general therefore:
The picture is further complicated as FHIR does allow an Encounter to be created with status "planned", however this is not recommended here and should normally be represented instead with an Appointment.
Further useful guidance can be found on the FHIR website, here:
https://hl7.org/fhir/R4/encounter.html#bnr
https://hl7.org/fhir/R4/appointment.html#statuses
https://hl7.org/fhir/R4/appointment.html#status-flow
significant set of mandatory fields are defined in order to properly describe an Encounter:
Status - this is already mandatory in FHIR. As noted above the use of "planned" is discouraged - use Appointment instead for this.
Class - this provides a categorisation, ie Emergency, Inpatient, Ambulatory. This should always be known, and vital for meaningful display purposes. We have defined a custom code list which replicates the standard list provided by Care Connect, and adds a codes to identify an "Encounter Grouping", and various types of ambulance/emergency service encounters. However it also enables the possibility of extending the list to cover a wider range of care settings if this is found to be necessary (please get in touch).
Subject - every encounter must be linked to a Patient (not a Group)
Participant - it is required to include EXACTLY ONE practitioner who has the "type" of "Primary Performer". This should be the main person responsible - someone who it would be useful to contact if further information is desired. (If this person changed during the course of the encounter then please pick just ONE to finally hold this key role, and demote the others to "participant")
Also included in the list of participants might be:
Participants can be given a "period" and this is optional. For regional sharing the most important thing is to see who has been involved with the patient, rather than to construct a forensic timeline of involvements. However this information might be useful in the case of a long Encounter with many brief involvements, and so may be provided if desired.
Period When the encounter occurred is vital to know. The start date/time is always mandatory, but as per the FHIR specification, the end date/time may be omitted if the encounter is ongoing.
In addition the following fields are "Must Support" - ie they must be populated if relevant and known. These largely relate to providing additional "clinical" detail about the Encounter - including links to related FHIR Resources such as the originating Appointment, the Condition, etc. These build up the rich dataset around an Encounter and are important to provide, but may not yet be available for an initial Encounter implementation.
Identifier - a Local Id should be provided, such that could be quoted if manually getting in touch to find out more
statusHistory - List of past encounter statuses.It is considered to be very important and useful to be able to see the progression and timeline of the encounter – from arrived, triaged, in-progress, etc
NB: The code for "Seen in Clinic" offers the ability to drill down into a long list of specific clinic types. However this overlaps to some extent with the purpose of the "Service Type" field - so it is sufficient here to populate simply "Seen in Clinic".
Service Type - this is perhaps one of the most important and useful fields about an Encounter as it describes the type of service - ie what the Encounter was "for".
Priority: This provides useful information about whether it was emergency, routine, elective, etc
Appointment: Link to the originating Appointment, if relevant
Reason Code: A long list of SNOMED codes to describe different reasons which may have led to the Encounter. (Note that this may duplicate to some extent information provided in a linked Appointment and/or Referral, but is seen as useful to pull through onto the Encounter itself also).
Reason Reference: Alternate element to provide reason details with reference to Condition / Procedure or Observation resource.
Diagnosis: Link to a Condition diagnosed as a result of the Encounter. Can obviously be provided only if the Condition FHIR Resource is also being offered. If populated then it is required to rank the Conditions, and to assign one the "role" of "Chief Complaint".
Hospitalization: To provide details of admission and discharge. As described above then, depending on circumstances, it might be actually populated fully, partially, or not at all. See below for further details of the fields contained
It is useful to understand the history of where the patient has been seen, so the status and period MUST be populated, and a history SHOULD be provided. (As noted above, a change of location does not in itself constitute a new Encounter, simply append to this list).
These provide valuable information which is important to populate. However it is expected that only one of the three will be populated, as relevant for the type of encounter
Other fields are optional and may be populated if known - on the understanding that not all data consumers will necessarily make use of them. Points of note include:
Episode of Care - again as described above, this may be used to link up a care pathway by pointing to an Episode of Care.
Based On: Link to the originating Referral, if relevant and implemented. This could be very useful information.
Length - the period is already provided, so this may appear to be duplication. However it is encouraged to populate if possible as it is useful for analytic purposes. If provided then the duration SHOULD be in minutes, and should reflect the time the patient is receiving direct care - eg not including the time the patient is waiting to be seen in clinic. (This provides a further distinction and greater analytical accuracy over-and-above the "period")
Part Of - as described above, this may be used to point to an overarching "EncounterGrouping" Encounter. No other complex structures or nesting are permitted.
extension:legalStatus - This UK Core extension extends the Encounter Resource to support the exchange of information relating to a patient’s legal status on admission or discharge.
#### Hospitalization Structure Within the Encounter sits the "Hospitalization" structure. This structure provides information about the admission and discharge. Therefore it is particularly important for a regional shared record - as this defines the touchpoints with other care providers.
Fields in the Hospitalization structure are as follows:
Admission Method - This extension provides a useful list of codes about the method of admission (eg Planned, A&E, transfer, etc)
Medically Safe For Discharge - This extension has been added to capture important information to assist with discharge planning and analysis. It contains a status code (ready, not ready, or unknown), plus the predicted and actual date when the patient is medically safe for discharge.
Note that Origin and Destination are likely to be external locations - please refer to guidance on the Location profile about use of References. For example the use of a Contained Resource may be appropriate.
Admit Source - Useful information about the type of place the patient came from (eg home, other NHS hospital, care home, etc)
Please note that the NHS Data Dictionary national codes for Source of Admission has been replaced with Admission Source. The current Valueset contains codes from both codesystems, however please use the new Interweave code system for new data provision projects.
Usage:
Description of Profiles, Differentials, Snapshots and how the different presentations work.
This structure is derived from UKCoreEncounter
| Name | Flags | Card. | Type | Description & Constraints |
|---|---|---|---|---|
 |
UKCoreEncounter | |||
  |
S | 0..1 | id | Logical id of this artifact |
  |
||||
   |
0..0 | |||
   |
S | 0..1 | id | Version specific identifier |
   |
S | 0..1 | instant | MANDATORY except in Contained Resources. When the resource version last changed. |
   |
S | 0..* | canonical(StructureDefinition) | Profiles this resource claims to conform to. Should list (i) this profile (ii) base profile for this resource. |
   |
0..* | Coding | DISCOURAGED - may not be honoured by Data Consumers | |
   |
0..* | Coding | Tags applied to this resource Slice: Unordered, Open by value:system | |
    |
S | 0..1 | Coding | MANDATORY except in Contained Resources. The Data Provider Id (and display text) of the system supplying the data |
     |
0..0 | |||
     |
1..1 | uri | Identity of the terminology system Fixed Value: https://fhir.interweavedigital.nhs.uk/Source | |
     |
0..0 | |||
     |
S | 1..1 | code | The Data Provider Id of the system supplying the data |
     |
S | 1..1 | string | Name of the system supplying the data |
    |
S | 0..1 | Coding | MANDATORY except in Contained Resources. The ODS Code (and display text) of the organisation responsible for the data |
     |
0..0 | |||
     |
1..1 | uri | Identity of the terminology system Fixed Value: https://fhir.interweavedigital.nhs.uk/Provenance | |
     |
0..0 | |||
     |
S | 1..1 | code | The ODS Code of the organisation responsible for the data |
     |
S | 1..1 | string | Name of the organisation supplying the data |
  |
0..1 | uri | DISCOURAGED - may not be honoured by Data Consumers | |
  |
0..1 | code | English is assumed (not currently a multi-lingual implementation) | |
  |
0..1 | Narrative | DISCOURAGED - the preferred approach is to offer structured data fields which a Data Consumer can then render and present in a manner most suited to its users | |
  |
Content/Rules for all slices | |||
   |
S | 0..1 | ExtensionUKCoreEmergencyCareDischargeStatus | An extension used indicate the status of a patient on discharge from an Emergency Care Department |
   |
S | 0..1 | CodeableConcept | Discharge destination of patients which have attended ED. URL: https://fhir.interweavedigital.nhs.uk/R4/StructureDefinition/Extension-Interweave-EDDischargeDestination Binding: InterweaveEDDischargeDestination (preferred) |
  |
0..* | Identifier | Identifier(s) by which this encounter is known. Slice: Unordered, Open by value:system | |
   |
Content/Rules for all slices | |||
    |
0..1 | Reference(InterweaveOrganization) | Organization that issued id (may be just text) | |
   |
S | 0..1 | Identifier | Identifier(s) by which this encounter is known. |
    |
S | 1..1 | uri | The namespace for the identifier value Fixed Value: https://fhir.interweavedigital.nhs.uk/Id/local-encounter-identifier |
    |
S | 1..1 | string | The Local encounter Identifier. Please prefix with ODS code plus period (XXX.) to ensure unique |
    |
0..0 | |||
  |
1..1 | code | arrived | triaged | in-progress | onleave | finished | cancelled | entered-in-error | unknown (Note: 'planned' is also possible, but normally represented instead as an Appointment) | |
  |
S | 0..* | BackboneElement | List of past encounter statuses |
  |
1..1 | Coding | Classification of the encounter. EXTENSIBLE on request, eg to cover other care settings Binding: InterweaveEncounterClass (required) | |
   |
1..1 | uri | Identity of the terminology system | |
   |
1..1 | code | Symbol in syntax defined by the system | |
   |
1..1 | string | Representation defined by the system | |
  |
0..0 | |||
  |
S | 0..1 | CodeableConcept | Specific type of encounter Binding: UK Core Encounter Type (required) |
   |
||||
    |
1..1 | uri | Identity of the terminology system | |
    |
1..1 | code | Symbol in syntax defined by the system | |
    |
1..1 | string | Representation defined by the system | |
  |
S | 0..1 | CodeableConcept | Specific type of service |
   |
||||
    |
1..1 | uri | Identity of the terminology system | |
    |
1..1 | code | Symbol in syntax defined by the system | |
    |
1..1 | string | Representation defined by the system | |
  |
S | 0..1 | CodeableConcept | Indicates the urgency of the encounter Binding: InterweaveEncounterPriority (required) |
   |
||||
    |
1..1 | uri | Identity of the terminology system | |
    |
1..1 | code | Symbol in syntax defined by the system | |
    |
1..1 | string | Representation defined by the system | |
  |
1..1 | Reference(InterweavePatient) | The patient (NOT group) present at the encounter | |
   |
1..1 | string | Reference to a resource (could be Contained) | |
   |
0..1 | Identifier | If relevant could include an id | |
   |
1..1 | string | Description of the referenced resource | |
  |
||||
   |
1..1 | string | Reference to a resource (could be Contained) | |
   |
0..1 | Identifier | If relevant could include an id | |
   |
0..1 | string | If relevant, description of the referenced resource | |
  |
1..* | BackboneElement | The list of people responsible for providing the service. | |
   |
S | 1..1 | CodeableConcept | Role of participant in encounter Binding: ParticipantType (required) |
    |
||||
     |
1..1 | uri | Identity of the terminology system | |
     |
1..1 | code | Symbol in syntax defined by the system | |
     |
1..1 | string | Representation defined by the system | |
   |
S | 1..1 | Reference(InterweavePractitioner) | Persons involved in the encounter other than the patient |
    |
1..1 | string | Reference to a resource (could be Contained) | |
    |
0..1 | Identifier | If relevant could include an id | |
    |
1..1 | string | Description of the referenced resource | |
  |
S | 0..1 | Reference(Appointment) | The appointment that scheduled this encounter |
   |
1..1 | string | Reference to a resource (could be Contained) | |
   |
0..1 | Identifier | If relevant could include an id | |
   |
0..1 | string | If relevant, description of the referenced resource | |
  |
S | 1..1 | Period | The start and end time of the encounter |
   |
S | 1..1 | dateTime | Starting time with inclusive boundary |
   |
S | 0..1 | dateTime | End time with inclusive boundary, if not ongoing |
  |
0..1 | Duration | Quantity of time the encounter lasted (less time absent). Please use minutes. | |
  |
||||
   |
||||
    |
1..1 | uri | Identity of the terminology system | |
    |
1..1 | code | Symbol in syntax defined by the system | |
    |
1..1 | string | Representation defined by the system | |
  |
S | 0..* | BackboneElement | The list of diagnosis relevant to this encounter Slice: Unordered, Open by value:use |
   |
Content/Rules for all slices | |||
    |
S | 1..1 | Reference(Condition | Procedure) | The diagnosis or procedure relevant to the encounter |
     |
1..1 | string | Reference to a resource (could be Contained) | |
     |
0..1 | Identifier | If relevant could include an id | |
     |
0..1 | string | If relevant, description of the referenced resource | |
    |
S | 1..1 | CodeableConcept | Role that this diagnosis has within the encounter (e.g. admission, billing, discharge …) Binding: DiagnosisRole (required) |
     |
||||
      |
1..1 | uri | Identity of the terminology system | |
      |
1..1 | code | Symbol in syntax defined by the system | |
      |
1..1 | string | Representation defined by the system | |
    |
S | 1..1 | positiveInt | Ranking of the diagnosis (for each role type) |
   |
S | 0..1 | BackboneElement | The list of diagnosis relevant to this encounter |
    |
0..1 | CodeableConcept | Role that this diagnosis has within the encounter (e.g. admission, billing, discharge …) Fixed Value: As shown | |
     |
1..1 | Coding | Code defined by a terminology system Fixed Value: (complex) | |
      |
1..1 | uri | Identity of the terminology system Fixed Value: http://terminology.hl7.org/CodeSystem/diagnosis-role | |
      |
1..1 | code | Symbol in syntax defined by the system Fixed Value: CC | |
      |
1..1 | string | Representation defined by the system Fixed Value: Chief complaint | |
  |
0..0 | |||
  |
S | 0..1 | BackboneElement | Details about the admission to a healthcare service |
   |
Content/Rules for all slices | |||
    |
S | 0..1 | ExtensionUKCoreAdmissionMethod | An extension to record how a patient was admitted to hospital |
    |
S | 0..1 | (Complex) | Medically Safe for Discharge URL: https://fhir.interweavedigital.nhs.uk/R4/StructureDefinition/Extension-Interweave-MedicallySafeForDischarge |
   |
0..1 | Reference(Location | Organization) | The location from which the patient came before admission. Useful to provide if possible, in particular to reference a 'site' if transfered from another institution. | |
    |
1..1 | string | Reference to a resource (could be Contained) | |
    |
0..1 | Identifier | If relevant could include an id | |
    |
1..1 | string | Description of the referenced resource | |
   |
S | 0..1 | CodeableConcept | From where patient was admitted (physician referral, transfer) Binding: InterweaveAdmissionSource (required) |
    |
||||
     |
1..1 | uri | Identity of the terminology system | |
     |
1..1 | code | Symbol in syntax defined by the system | |
     |
1..1 | string | Representation defined by the system | |
   |
0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing | |
   |
0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing | |
   |
0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing | |
   |
S | 0..1 | Reference(Location | Organization) | Location to which the patient is discharged. Important to provide if known to support discharge planning, and/or to reference a 'site' if transfered to another institution. |
    |
1..1 | string | Reference to a resource (could be Contained) | |
    |
0..1 | Identifier | If relevant could include an id | |
    |
1..1 | string | Description of the referenced resource | |
   |
S | 0..1 | CodeableConcept | Category or kind of location after discharge Binding: InterweaveDischargeDestination (required) |
    |
||||
     |
1..1 | uri | Identity of the terminology system | |
     |
1..1 | code | Symbol in syntax defined by the system | |
     |
1..1 | string | Representation defined by the system | |
  |
S | 0..* | BackboneElement | Location the encounter takes place (at Ward level) |
   |
S | 1..1 | Reference(Location) | Location the encounter takes place |
    |
1..1 | string | Reference to a resource (could be Contained) | |
    |
0..1 | Identifier | If relevant could include an id | |
    |
1..1 | string | Description of the referenced resource | |
   |
S | 1..1 | code | planned | active | reserved | completed |
   |
S | 1..1 | Period | Time period during which the patient was present at the location |
  |
0..1 | Reference(Organization) | DISCOURAGED: This is instead covered via the provenance tags | |
  |
0..1 | Reference(InterweaveEncounterGrouping) | Another Encounter this encounter is part of | |
   |
1..1 | string | Reference to a resource (could be Contained) | |
   |
0..1 | Identifier | If relevant could include an id | |
   |
0..1 | string | If relevant, description of the referenced resource | |
 Documentation for this format Documentation for this format | ||||
| Path | Conformance | ValueSet | URI |
| Encounter.class | required | InterweaveEncounterClasshttps://fhir.interweavedigital.nhs.uk/R4/ValueSet/Interweave-EncounterClassfrom this IG | |
| Encounter.type | required | UKCoreEncounterTypehttps://fhir.hl7.org.uk/ValueSet/UKCore-EncounterTypefrom this IG | |
| Encounter.priority | required | InterweaveEncounterPriorityhttps://fhir.interweavedigital.nhs.uk/R4/ValueSet/Interweave-EncounterPriorityfrom this IG | |
| Encounter.participant.type | required | ParticipantTypehttp://hl7.org/fhir/ValueSet/encounter-participant-typefrom the FHIR Standard | |
| Encounter.diagnosis.use | required | DiagnosisRolehttp://hl7.org/fhir/ValueSet/diagnosis-rolefrom the FHIR Standard | |
| Encounter.hospitalization.admitSource | required | InterweaveAdmissionSourcehttps://fhir.interweavedigital.nhs.uk/R4/ValueSet/Interweave-AdmissionSourcefrom this IG | |
| Encounter.hospitalization.dischargeDisposition | required | InterweaveDischargeDestinationhttps://fhir.interweavedigital.nhs.uk/R4/ValueSet/Interweave-DischargeDestinationfrom this IG |
| Name | Flags | Card. | Type | Description & Constraints | ||||
|---|---|---|---|---|---|---|---|---|
 |
0..* | UKCoreEncounter | An interaction during which services are provided to the patient | |||||
  |
SΣ | 0..1 | id | Logical id of this artifact | ||||
  |
Σ | 0..1 | Meta | Metadata about the resource | ||||
   |
SΣ | 0..1 | id | Version specific identifier | ||||
   |
SΣ | 0..1 | instant | MANDATORY except in Contained Resources. When the resource version last changed. | ||||
   |
SΣ | 0..* | canonical(StructureDefinition) | Profiles this resource claims to conform to. Should list (i) this profile (ii) base profile for this resource. | ||||
   |
Σ | 0..* | Coding | DISCOURAGED - may not be honoured by Data Consumers Binding: All Security Labels (extensible): Security Labels from the Healthcare Privacy and Security Classification System. | ||||
   |
Σ | 0..* | Coding | Tags applied to this resource Slice: Unordered, Open by value:system Binding: CommonTags (example): Codes that represent various types of tags, commonly workflow-related; e.g. "Needs review by Dr. Jones". | ||||
    |
SΣ | 0..1 | Coding | MANDATORY except in Contained Resources. The Data Provider Id (and display text) of the system supplying the data Binding: CommonTags (example): Codes that represent various types of tags, commonly workflow-related; e.g. "Needs review by Dr. Jones". | ||||
     |
Σ | 1..1 | uri | Identity of the terminology system Fixed Value: https://fhir.interweavedigital.nhs.uk/Source | ||||
     |
SΣ | 1..1 | code | The Data Provider Id of the system supplying the data | ||||
     |
SΣ | 1..1 | string | Name of the system supplying the data | ||||
    |
SΣ | 0..1 | Coding | MANDATORY except in Contained Resources. The ODS Code (and display text) of the organisation responsible for the data Binding: CommonTags (example): Codes that represent various types of tags, commonly workflow-related; e.g. "Needs review by Dr. Jones". | ||||
     |
Σ | 1..1 | uri | Identity of the terminology system Fixed Value: https://fhir.interweavedigital.nhs.uk/Provenance | ||||
     |
SΣ | 1..1 | code | The ODS Code of the organisation responsible for the data | ||||
     |
SΣ | 1..1 | string | Name of the organisation supplying the data | ||||
  |
?!Σ | 0..1 | uri | DISCOURAGED - may not be honoured by Data Consumers | ||||
  |
0..1 | code | English is assumed (not currently a multi-lingual implementation) Binding: CommonLanguages (preferred): A human language.
| |||||
  |
0..1 | Narrative | DISCOURAGED - the preferred approach is to offer structured data fields which a Data Consumer can then render and present in a manner most suited to its users | |||||
  |
Content/Rules for all slices | |||||||
   |
0..1 | CodeableConcept | An extension to support the method of discharge from a hospital. URL: https://fhir.hl7.org.uk/StructureDefinition/Extension-UKCore-DischargeMethod Binding: UK Core Discharge Method (extensible): The method by which a patient was discharged from hospital | |||||
   |
S | 0..1 | CodeableConcept | An extension used indicate the status of a patient on discharge from an Emergency Care Department URL: https://fhir.hl7.org.uk/StructureDefinition/Extension-UKCore-EmergencyCareDischargeStatus Binding: UK Core Emergency Care Discharge Status (preferred): The status of a patient on discharge from an Emergency Care Department | ||||
   |
0..* | (Complex) | Information relating to a patient's legal status on admission or discharge. URL: https://fhir.hl7.org.uk/StructureDefinition/Extension-UKCore-LegalStatus | |||||
   |
0..1 | CodeableConcept | An extension to support the outcome of an Outpatient attendance. URL: https://fhir.hl7.org.uk/StructureDefinition/Extension-UKCore-OutcomeOfAttendance Binding: UK Core Outcome Of Attendance (extensible): The outcome of an outpatient attendance | |||||
   |
S | 0..1 | CodeableConcept | Discharge destination of patients which have attended ED. URL: https://fhir.interweavedigital.nhs.uk/R4/StructureDefinition/Extension-Interweave-EDDischargeDestination Binding: InterweaveEDDischargeDestination (preferred) | ||||
  |
?! | 0..* | Extension | Extensions that cannot be ignored | ||||
  |
SΣ | 0..* | Identifier | Identifier(s) by which this encounter is known. Slice: Unordered, Open by value:system | ||||
   |
Content/Rules for all slices | |||||||
    |
?!Σ | 0..1 | code | usual | official | temp | secondary | old (If known) Binding: IdentifierUse (required): Identifies the purpose for this identifier, if known . | ||||
    |
Σ | 0..1 | Reference(InterweaveOrganization) | Organization that issued id (may be just text) | ||||
   |
SΣ | 0..1 | Identifier | Identifier(s) by which this encounter is known. | ||||
    |
?!Σ | 0..1 | code | usual | official | temp | secondary | old (If known) Binding: IdentifierUse (required): Identifies the purpose for this identifier, if known . | ||||
    |
SΣ | 1..1 | uri | The namespace for the identifier value Fixed Value: https://fhir.interweavedigital.nhs.uk/Id/local-encounter-identifier | ||||
    |
SΣ | 1..1 | string | The Local encounter Identifier. Please prefix with ODS code plus period (XXX.) to ensure unique Example General: 123456 | ||||
  |
?!SΣ | 1..1 | code | arrived | triaged | in-progress | onleave | finished | cancelled | entered-in-error | unknown (Note: 'planned' is also possible, but normally represented instead as an Appointment) Binding: EncounterStatus (required): Current state of the encounter. | ||||
  |
S | 0..* | BackboneElement | List of past encounter statuses | ||||
   |
?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
   |
1..1 | code | planned | arrived | triaged | in-progress | onleave | finished | cancelled + Binding: EncounterStatus (required): Current state of the encounter. | |||||
   |
1..1 | Period | The time that the episode was in the specified status | |||||
  |
SΣ | 1..1 | Coding | Classification of the encounter. EXTENSIBLE on request, eg to cover other care settings Binding: InterweaveEncounterClass (required) | ||||
   |
Σ | 1..1 | uri | Identity of the terminology system | ||||
   |
Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
   |
Σ | 1..1 | string | Representation defined by the system | ||||
  |
SΣ | 0..1 | CodeableConcept | Specific type of encounter Binding: UK Core Encounter Type (required) | ||||
  |
SΣ | 0..1 | CodeableConcept | Specific type of service Binding: UK Core Care Setting Type (preferred): Any code from the SNOMED CT UK Refset with fully specified name 'Services simple reference set (foundation metadata concept)' with Refset Id 1127531000000102. | ||||
  |
S | 0..1 | CodeableConcept | Indicates the urgency of the encounter Binding: InterweaveEncounterPriority (required) | ||||
  |
SΣ | 1..1 | Reference(InterweavePatient) | The patient (NOT group) present at the encounter | ||||
   |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
   |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
   |
Σ | 1..1 | string | Description of the referenced resource | ||||
  |
SΣ | 1..* | BackboneElement | The list of people responsible for providing the service. | ||||
   |
?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
   |
SΣ | 1..1 | CodeableConcept | Role of participant in encounter Binding: ParticipantType (required) | ||||
   |
SΣ | 1..1 | Reference(InterweavePractitioner) | Persons involved in the encounter other than the patient | ||||
    |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
    |
Σ | 1..1 | string | Description of the referenced resource | ||||
  |
SΣ | 0..1 | Reference(Appointment) | The appointment that scheduled this encounter | ||||
   |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
   |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
   |
Σ | 0..1 | string | If relevant, description of the referenced resource | ||||
  |
S | 1..1 | Period | The start and end time of the encounter | ||||
   |
SΣC | 1..1 | dateTime | Starting time with inclusive boundary | ||||
   |
SΣC | 0..1 | dateTime | End time with inclusive boundary, if not ongoing | ||||
  |
0..1 | Duration | Quantity of time the encounter lasted (less time absent). Please use minutes. | |||||
  |
SΣ | 0..* | CodeableConcept | Reason the encounter takes place, expressed as a code. For admissions, this can be used for a coded admission diagnosis. Binding: EncounterReasonCodes (preferred): Reason why the encounter takes place. | ||||
  |
SΣ | 0..* | Reference(Condition | Procedure | Observation | ImmunizationRecommendation) | Reason the encounter takes place, expressed as a reference to a Condition, Procedure, Observation, or ImmunizationRecommendation. | ||||
  |
SΣ | 0..* | BackboneElement | The list of diagnosis relevant to this encounter Slice: Unordered, Open by value:use | ||||
   |
Content/Rules for all slices | |||||||
    |
?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
    |
SΣ | 1..1 | Reference(Condition | Procedure) | The diagnosis or procedure relevant to the encounter | ||||
     |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
     |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
     |
Σ | 0..1 | string | If relevant, description of the referenced resource | ||||
    |
S | 1..1 | CodeableConcept | Role that this diagnosis has within the encounter (e.g. admission, billing, discharge …) Binding: DiagnosisRole (required) | ||||
    |
S | 1..1 | positiveInt | Ranking of the diagnosis (for each role type) | ||||
   |
SΣ | 0..1 | BackboneElement | The list of diagnosis relevant to this encounter | ||||
    |
?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
    |
Σ | 1..1 | Reference(Condition | Procedure) | The diagnosis or procedure relevant to the encounter | ||||
    |
0..1 | CodeableConcept | Role that this diagnosis has within the encounter (e.g. admission, billing, discharge …) Binding: DiagnosisRole (preferred): The type of diagnosis this condition represents. Fixed Value: As shown | |||||
     |
0..0 | string | Unique id for inter-element referencing | |||||
     |
0..0 | Extension | Additional content defined by implementations | |||||
     |
1..1 | Coding | Code defined by a terminology system Fixed Value: (complex) | |||||
      |
0..0 | string | Unique id for inter-element referencing | |||||
      |
0..0 | Extension | Additional content defined by implementations | |||||
      |
1..1 | uri | Identity of the terminology system Fixed Value: http://terminology.hl7.org/CodeSystem/diagnosis-role | |||||
      |
0..0 | string | Version of the system - if relevant | |||||
      |
1..1 | code | Symbol in syntax defined by the system Fixed Value: CC | |||||
      |
1..1 | string | Representation defined by the system Fixed Value: Chief complaint | |||||
      |
0..0 | boolean | If this coding was chosen directly by the user | |||||
     |
0..0 | string | Plain text representation of the concept | |||||
  |
S | 0..1 | BackboneElement | Details about the admission to a healthcare service | ||||
   |
Content/Rules for all slices | |||||||
    |
S | 0..1 | CodeableConcept | An extension to record how a patient was admitted to hospital URL: https://fhir.hl7.org.uk/StructureDefinition/Extension-UKCore-AdmissionMethod Binding: UK Core Admission Method (extensible): The method by which a patient was admitted to hospital | ||||
    |
S | 0..1 | (Complex) | Medically Safe for Discharge URL: https://fhir.interweavedigital.nhs.uk/R4/StructureDefinition/Extension-Interweave-MedicallySafeForDischarge | ||||
   |
?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
   |
0..1 | Reference(Location | Organization) | The location from which the patient came before admission. Useful to provide if possible, in particular to reference a 'site' if transfered from another institution. | |||||
    |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
    |
Σ | 1..1 | string | Description of the referenced resource | ||||
   |
S | 0..1 | CodeableConcept | From where patient was admitted (physician referral, transfer) Binding: InterweaveAdmissionSource (required) | ||||
   |
0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing Binding: Diet (example): Medical, cultural or ethical food preferences to help with catering requirements. | |||||
   |
0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing Binding: SpecialCourtesy (preferred): Special courtesies. | |||||
   |
0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing Binding: SpecialArrangements (preferred): Special arrangements. | |||||
   |
S | 0..1 | Reference(Location | Organization) | Location to which the patient is discharged. Important to provide if known to support discharge planning, and/or to reference a 'site' if transfered to another institution. | ||||
    |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
    |
Σ | 1..1 | string | Description of the referenced resource | ||||
   |
S | 0..1 | CodeableConcept | Category or kind of location after discharge Binding: InterweaveDischargeDestination (required) | ||||
  |
S | 0..* | BackboneElement | Location the encounter takes place (at Ward level) | ||||
   |
?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
   |
S | 1..1 | Reference(Location) | Location the encounter takes place | ||||
    |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
    |
Σ | 1..1 | string | Description of the referenced resource | ||||
   |
S | 1..1 | code | planned | active | reserved | completed Binding: EncounterLocationStatus (required): The status of the location. | ||||
   |
S | 1..1 | Period | Time period during which the patient was present at the location | ||||
  |
0..1 | Reference(Organization) | DISCOURAGED: This is instead covered via the provenance tags | |||||
  |
0..1 | Reference(InterweaveEncounterGrouping) | Another Encounter this encounter is part of | |||||
   |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
   |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
   |
Σ | 0..1 | string | If relevant, description of the referenced resource | ||||
 Documentation for this format Documentation for this format | ||||||||
| Path | Conformance | ValueSet / Code | URI | |||
| Encounter.meta.security | extensible | All Security Labelshttp://hl7.org/fhir/ValueSet/security-labelsfrom the FHIR Standard | ||||
| Encounter.meta.tag | example | CommonTagshttp://hl7.org/fhir/ValueSet/common-tagsfrom the FHIR Standard | ||||
| Encounter.meta.tag:Source | example | CommonTagshttp://hl7.org/fhir/ValueSet/common-tagsfrom the FHIR Standard | ||||
| Encounter.meta.tag:Provenance | example | CommonTagshttp://hl7.org/fhir/ValueSet/common-tagsfrom the FHIR Standard | ||||
| Encounter.language | preferred | CommonLanguages
http://hl7.org/fhir/ValueSet/languagesfrom the FHIR Standard | ||||
| Encounter.identifier.use | required | IdentifierUsehttp://hl7.org/fhir/ValueSet/identifier-use|4.0.1from the FHIR Standard | ||||
| Encounter.identifier:localIdentifier.use | required | IdentifierUsehttp://hl7.org/fhir/ValueSet/identifier-use|4.0.1from the FHIR Standard | ||||
| Encounter.status | required | EncounterStatushttp://hl7.org/fhir/ValueSet/encounter-status|4.0.1from the FHIR Standard | ||||
| Encounter.statusHistory.status | required | EncounterStatushttp://hl7.org/fhir/ValueSet/encounter-status|4.0.1from the FHIR Standard | ||||
| Encounter.class | required | InterweaveEncounterClasshttps://fhir.interweavedigital.nhs.uk/R4/ValueSet/Interweave-EncounterClassfrom this IG | ||||
| Encounter.classHistory.class | extensible | ActEncounterCodehttp://terminology.hl7.org/ValueSet/v3-ActEncounterCode | ||||
| Encounter.type | required | UKCoreEncounterTypehttps://fhir.hl7.org.uk/ValueSet/UKCore-EncounterTypefrom this IG | ||||
| Encounter.serviceType | preferred | UKCoreCareSettingTypehttps://fhir.hl7.org.uk/ValueSet/UKCore-CareSettingTypefrom this IG | ||||
| Encounter.priority | required | InterweaveEncounterPriorityhttps://fhir.interweavedigital.nhs.uk/R4/ValueSet/Interweave-EncounterPriorityfrom this IG | ||||
| Encounter.participant.type | required | ParticipantTypehttp://hl7.org/fhir/ValueSet/encounter-participant-typefrom the FHIR Standard | ||||
| Encounter.reasonCode | preferred | EncounterReasonCodeshttp://hl7.org/fhir/ValueSet/encounter-reasonfrom the FHIR Standard | ||||
| Encounter.diagnosis.use | required | DiagnosisRolehttp://hl7.org/fhir/ValueSet/diagnosis-rolefrom the FHIR Standard | ||||
| Encounter.diagnosis:chiefComplaint.use | preferred | Fixed Value: CC("Chief complaint")http://hl7.org/fhir/ValueSet/diagnosis-rolefrom the FHIR Standard | ||||
| Encounter.hospitalization.admitSource | required | InterweaveAdmissionSourcehttps://fhir.interweavedigital.nhs.uk/R4/ValueSet/Interweave-AdmissionSourcefrom this IG | ||||
| Encounter.hospitalization.dietPreference | example | Diethttp://hl7.org/fhir/ValueSet/encounter-dietfrom the FHIR Standard | ||||
| Encounter.hospitalization.specialCourtesy | preferred | SpecialCourtesyhttp://hl7.org/fhir/ValueSet/encounter-special-courtesyfrom the FHIR Standard | ||||
| Encounter.hospitalization.specialArrangement | preferred | SpecialArrangementshttp://hl7.org/fhir/ValueSet/encounter-special-arrangementsfrom the FHIR Standard | ||||
| Encounter.hospitalization.dischargeDisposition | required | InterweaveDischargeDestinationhttps://fhir.interweavedigital.nhs.uk/R4/ValueSet/Interweave-DischargeDestinationfrom this IG | ||||
| Encounter.location.status | required | EncounterLocationStatushttp://hl7.org/fhir/ValueSet/encounter-location-status|4.0.1from the FHIR Standard |
| Id | Grade | Path(s) | Details | Requirements |
| dom-2 | error | Encounter | If the resource is contained in another resource, it SHALL NOT contain nested Resources : contained.contained.empty() | |
| dom-3 | error | Encounter | If the resource is contained in another resource, it SHALL be referred to from elsewhere in the resource or SHALL refer to the containing resource : contained.where((('#'+id in (%resource.descendants().reference | %resource.descendants().as(canonical) | %resource.descendants().as(uri) | %resource.descendants().as(url))) or descendants().where(reference = '#').exists() or descendants().where(as(canonical) = '#').exists() or descendants().where(as(canonical) = '#').exists()).not()).trace('unmatched', id).empty() | |
| dom-4 | error | Encounter | If a resource is contained in another resource, it SHALL NOT have a meta.versionId or a meta.lastUpdated : contained.meta.versionId.empty() and contained.meta.lastUpdated.empty() | |
| dom-5 | error | Encounter | If a resource is contained in another resource, it SHALL NOT have a security label : contained.meta.security.empty() | |
| dom-6 | best practice | Encounter | A resource should have narrative for robust management : text.`div`.exists() | |
| ele-1 | error | **ALL** elements | All FHIR elements must have a @value or children : hasValue() or (children().count() > id.count()) | |
| ext-1 | error | **ALL** extensions | Must have either extensions or value[x], not both : extension.exists() != value.exists() |
| Name | Flags | Card. | Type | Description & Constraints | ||||
|---|---|---|---|---|---|---|---|---|
 |
0..* | UKCoreEncounter | An interaction during which services are provided to the patient | |||||
  |
SΣ | 0..1 | id | Logical id of this artifact | ||||
  |
Σ | 0..1 | Meta | Metadata about the resource | ||||
   |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
   |
SΣ | 0..1 | id | Version specific identifier | ||||
   |
SΣ | 0..1 | instant | MANDATORY except in Contained Resources. When the resource version last changed. | ||||
   |
Σ | 0..1 | uri | Identifies where the resource comes from | ||||
   |
SΣ | 0..* | canonical(StructureDefinition) | Profiles this resource claims to conform to. Should list (i) this profile (ii) base profile for this resource. | ||||
   |
Σ | 0..* | Coding | DISCOURAGED - may not be honoured by Data Consumers Binding: All Security Labels (extensible): Security Labels from the Healthcare Privacy and Security Classification System. | ||||
   |
Σ | 0..* | Coding | Tags applied to this resource Slice: Unordered, Open by value:system Binding: CommonTags (example): Codes that represent various types of tags, commonly workflow-related; e.g. "Needs review by Dr. Jones". | ||||
    |
SΣ | 0..1 | Coding | MANDATORY except in Contained Resources. The Data Provider Id (and display text) of the system supplying the data Binding: CommonTags (example): Codes that represent various types of tags, commonly workflow-related; e.g. "Needs review by Dr. Jones". | ||||
     |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
     |
Σ | 1..1 | uri | Identity of the terminology system Fixed Value: https://fhir.interweavedigital.nhs.uk/Source | ||||
     |
SΣ | 1..1 | code | The Data Provider Id of the system supplying the data | ||||
     |
SΣ | 1..1 | string | Name of the system supplying the data | ||||
     |
Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
    |
SΣ | 0..1 | Coding | MANDATORY except in Contained Resources. The ODS Code (and display text) of the organisation responsible for the data Binding: CommonTags (example): Codes that represent various types of tags, commonly workflow-related; e.g. "Needs review by Dr. Jones". | ||||
     |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
     |
Σ | 1..1 | uri | Identity of the terminology system Fixed Value: https://fhir.interweavedigital.nhs.uk/Provenance | ||||
     |
SΣ | 1..1 | code | The ODS Code of the organisation responsible for the data | ||||
     |
SΣ | 1..1 | string | Name of the organisation supplying the data | ||||
     |
Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
  |
?!Σ | 0..1 | uri | DISCOURAGED - may not be honoured by Data Consumers | ||||
  |
0..1 | code | English is assumed (not currently a multi-lingual implementation) Binding: CommonLanguages (preferred): A human language.
| |||||
  |
0..1 | Narrative | DISCOURAGED - the preferred approach is to offer structured data fields which a Data Consumer can then render and present in a manner most suited to its users | |||||
  |
0..* | Resource | Contained, inline Resources | |||||
  |
0..* | Extension | Extension Slice: Unordered, Open by value:url | |||||
   |
0..1 | CodeableConcept | An extension to support the method of discharge from a hospital. URL: https://fhir.hl7.org.uk/StructureDefinition/Extension-UKCore-DischargeMethod Binding: UK Core Discharge Method (extensible): The method by which a patient was discharged from hospital | |||||
   |
S | 0..1 | CodeableConcept | An extension used indicate the status of a patient on discharge from an Emergency Care Department URL: https://fhir.hl7.org.uk/StructureDefinition/Extension-UKCore-EmergencyCareDischargeStatus Binding: UK Core Emergency Care Discharge Status (preferred): The status of a patient on discharge from an Emergency Care Department | ||||
   |
0..* | (Complex) | Information relating to a patient's legal status on admission or discharge. URL: https://fhir.hl7.org.uk/StructureDefinition/Extension-UKCore-LegalStatus | |||||
   |
0..1 | CodeableConcept | An extension to support the outcome of an Outpatient attendance. URL: https://fhir.hl7.org.uk/StructureDefinition/Extension-UKCore-OutcomeOfAttendance Binding: UK Core Outcome Of Attendance (extensible): The outcome of an outpatient attendance | |||||
   |
S | 0..1 | CodeableConcept | Discharge destination of patients which have attended ED. URL: https://fhir.interweavedigital.nhs.uk/R4/StructureDefinition/Extension-Interweave-EDDischargeDestination Binding: InterweaveEDDischargeDestination (preferred) | ||||
  |
?! | 0..* | Extension | Extensions that cannot be ignored | ||||
  |
SΣ | 0..* | Identifier | Identifier(s) by which this encounter is known. Slice: Unordered, Open by value:system | ||||
   |
Content/Rules for all slices | |||||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
    |
?!Σ | 0..1 | code | usual | official | temp | secondary | old (If known) Binding: IdentifierUse (required): Identifies the purpose for this identifier, if known . | ||||
    |
Σ | 0..1 | CodeableConcept | Description of identifier Binding: Identifier Type Codes (extensible): A coded type for an identifier that can be used to determine which identifier to use for a specific purpose. | ||||
    |
Σ | 0..1 | uri | The namespace for the identifier value Example General: http://www.acme.com/identifiers/patient | ||||
    |
Σ | 0..1 | string | The value that is unique Example General: 123456 | ||||
    |
Σ | 0..1 | Period | Time period when id is/was valid for use | ||||
    |
Σ | 0..1 | Reference(InterweaveOrganization) | Organization that issued id (may be just text) | ||||
   |
SΣ | 0..1 | Identifier | Identifier(s) by which this encounter is known. | ||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
    |
?!Σ | 0..1 | code | usual | official | temp | secondary | old (If known) Binding: IdentifierUse (required): Identifies the purpose for this identifier, if known . | ||||
    |
Σ | 0..1 | CodeableConcept | Description of identifier Binding: Identifier Type Codes (extensible): A coded type for an identifier that can be used to determine which identifier to use for a specific purpose. | ||||
    |
SΣ | 1..1 | uri | The namespace for the identifier value Fixed Value: https://fhir.interweavedigital.nhs.uk/Id/local-encounter-identifier | ||||
    |
SΣ | 1..1 | string | The Local encounter Identifier. Please prefix with ODS code plus period (XXX.) to ensure unique Example General: 123456 | ||||
    |
Σ | 0..1 | Reference(Organization) | Organization that issued id (may be just text) | ||||
  |
?!SΣ | 1..1 | code | arrived | triaged | in-progress | onleave | finished | cancelled | entered-in-error | unknown (Note: 'planned' is also possible, but normally represented instead as an Appointment) Binding: EncounterStatus (required): Current state of the encounter. | ||||
  |
S | 0..* | BackboneElement | List of past encounter statuses | ||||
   |
0..1 | string | Unique id for inter-element referencing | |||||
   |
0..* | Extension | Additional content defined by implementations | |||||
   |
?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
   |
1..1 | code | planned | arrived | triaged | in-progress | onleave | finished | cancelled + Binding: EncounterStatus (required): Current state of the encounter. | |||||
   |
1..1 | Period | The time that the episode was in the specified status | |||||
  |
SΣ | 1..1 | Coding | Classification of the encounter. EXTENSIBLE on request, eg to cover other care settings Binding: InterweaveEncounterClass (required) | ||||
   |
0..1 | string | Unique id for inter-element referencing | |||||
   |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
   |
Σ | 1..1 | uri | Identity of the terminology system | ||||
   |
Σ | 0..1 | string | Version of the system - if relevant | ||||
   |
Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
   |
Σ | 1..1 | string | Representation defined by the system | ||||
   |
Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
  |
SΣ | 0..1 | CodeableConcept | Specific type of encounter Binding: UK Core Encounter Type (required) | ||||
   |
0..1 | string | Unique id for inter-element referencing | |||||
   |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
   |
Σ | 0..* | Coding | Code defined by a terminology system | ||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
    |
Σ | 1..1 | uri | Identity of the terminology system | ||||
    |
Σ | 0..1 | string | Version of the system - if relevant | ||||
    |
Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
    |
Σ | 1..1 | string | Representation defined by the system | ||||
    |
Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
   |
Σ | 0..1 | string | Plain text representation of the concept | ||||
  |
SΣ | 0..1 | CodeableConcept | Specific type of service Binding: UK Core Care Setting Type (preferred): Any code from the SNOMED CT UK Refset with fully specified name 'Services simple reference set (foundation metadata concept)' with Refset Id 1127531000000102. | ||||
   |
0..1 | string | Unique id for inter-element referencing | |||||
   |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
   |
Σ | 0..* | Coding | Code defined by a terminology system | ||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
    |
Σ | 1..1 | uri | Identity of the terminology system | ||||
    |
Σ | 0..1 | string | Version of the system - if relevant | ||||
    |
Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
    |
Σ | 1..1 | string | Representation defined by the system | ||||
    |
Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
   |
Σ | 0..1 | string | Plain text representation of the concept | ||||
  |
S | 0..1 | CodeableConcept | Indicates the urgency of the encounter Binding: InterweaveEncounterPriority (required) | ||||
   |
0..1 | string | Unique id for inter-element referencing | |||||
   |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
   |
Σ | 0..* | Coding | Code defined by a terminology system | ||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
    |
Σ | 1..1 | uri | Identity of the terminology system | ||||
    |
Σ | 0..1 | string | Version of the system - if relevant | ||||
    |
Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
    |
Σ | 1..1 | string | Representation defined by the system | ||||
    |
Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
   |
Σ | 0..1 | string | Plain text representation of the concept | ||||
  |
SΣ | 1..1 | Reference(InterweavePatient) | The patient (NOT group) present at the encounter | ||||
   |
0..1 | string | Unique id for inter-element referencing | |||||
   |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
   |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
   |
Σ | 0..1 | uri | Type the reference refers to (e.g. "Patient") Binding: ResourceType (extensible): Aa resource (or, for logical models, the URI of the logical model). | ||||
   |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
   |
Σ | 1..1 | string | Description of the referenced resource | ||||
  |
Σ | 0..* | Reference(EpisodeOfCare) | Episode(s) of care that this encounter should be recorded against | ||||
  |
0..* | Reference(ServiceRequest) | The ServiceRequest that initiated this encounter | |||||
   |
0..1 | string | Unique id for inter-element referencing | |||||
   |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
   |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
   |
Σ | 0..1 | uri | Type the reference refers to (e.g. "Patient") Binding: ResourceType (extensible): Aa resource (or, for logical models, the URI of the logical model). | ||||
   |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
   |
Σ | 0..1 | string | If relevant, description of the referenced resource | ||||
  |
SΣ | 1..* | BackboneElement | The list of people responsible for providing the service. | ||||
   |
0..1 | string | Unique id for inter-element referencing | |||||
   |
0..* | Extension | Additional content defined by implementations | |||||
   |
?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
   |
SΣ | 1..1 | CodeableConcept | Role of participant in encounter Binding: ParticipantType (required) | ||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
    |
Σ | 0..* | Coding | Code defined by a terminology system | ||||
     |
0..1 | string | Unique id for inter-element referencing | |||||
     |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
     |
Σ | 1..1 | uri | Identity of the terminology system | ||||
     |
Σ | 0..1 | string | Version of the system - if relevant | ||||
     |
Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
     |
Σ | 1..1 | string | Representation defined by the system | ||||
     |
Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
    |
Σ | 0..1 | string | Plain text representation of the concept | ||||
   |
0..1 | Period | Period of time during the encounter that the participant participated | |||||
   |
SΣ | 1..1 | Reference(InterweavePractitioner) | Persons involved in the encounter other than the patient | ||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
    |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    |
Σ | 0..1 | uri | Type the reference refers to (e.g. "Patient") Binding: ResourceType (extensible): Aa resource (or, for logical models, the URI of the logical model). | ||||
    |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
    |
Σ | 1..1 | string | Description of the referenced resource | ||||
  |
SΣ | 0..1 | Reference(Appointment) | The appointment that scheduled this encounter | ||||
   |
0..1 | string | Unique id for inter-element referencing | |||||
   |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
   |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
   |
Σ | 0..1 | uri | Type the reference refers to (e.g. "Patient") Binding: ResourceType (extensible): Aa resource (or, for logical models, the URI of the logical model). | ||||
   |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
   |
Σ | 0..1 | string | If relevant, description of the referenced resource | ||||
  |
S | 1..1 | Period | The start and end time of the encounter | ||||
   |
0..1 | string | Unique id for inter-element referencing | |||||
   |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
   |
SΣC | 1..1 | dateTime | Starting time with inclusive boundary | ||||
   |
SΣC | 0..1 | dateTime | End time with inclusive boundary, if not ongoing | ||||
  |
0..1 | Duration | Quantity of time the encounter lasted (less time absent). Please use minutes. | |||||
  |
SΣ | 0..* | CodeableConcept | Reason the encounter takes place, expressed as a code. For admissions, this can be used for a coded admission diagnosis. Binding: EncounterReasonCodes (preferred): Reason why the encounter takes place. | ||||
   |
0..1 | string | Unique id for inter-element referencing | |||||
   |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
   |
Σ | 0..* | Coding | Code defined by a terminology system | ||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
    |
Σ | 1..1 | uri | Identity of the terminology system | ||||
    |
Σ | 0..1 | string | Version of the system - if relevant | ||||
    |
Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
    |
Σ | 1..1 | string | Representation defined by the system | ||||
    |
Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
   |
Σ | 0..1 | string | Plain text representation of the concept | ||||
  |
SΣ | 0..* | Reference(Condition | Procedure | Observation | ImmunizationRecommendation) | Reason the encounter takes place, expressed as a reference to a Condition, Procedure, Observation, or ImmunizationRecommendation. | ||||
  |
SΣ | 0..* | BackboneElement | The list of diagnosis relevant to this encounter Slice: Unordered, Open by value:use | ||||
   |
Content/Rules for all slices | |||||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations | |||||
    |
?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
    |
SΣ | 1..1 | Reference(Condition | Procedure) | The diagnosis or procedure relevant to the encounter | ||||
     |
0..1 | string | Unique id for inter-element referencing | |||||
     |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
     |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
     |
Σ | 0..1 | uri | Type the reference refers to (e.g. "Patient") Binding: ResourceType (extensible): Aa resource (or, for logical models, the URI of the logical model). | ||||
     |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
     |
Σ | 0..1 | string | If relevant, description of the referenced resource | ||||
    |
S | 1..1 | CodeableConcept | Role that this diagnosis has within the encounter (e.g. admission, billing, discharge …) Binding: DiagnosisRole (required) | ||||
     |
0..1 | string | Unique id for inter-element referencing | |||||
     |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
     |
Σ | 0..* | Coding | Code defined by a terminology system | ||||
      |
0..1 | string | Unique id for inter-element referencing | |||||
      |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
      |
Σ | 1..1 | uri | Identity of the terminology system | ||||
      |
Σ | 0..1 | string | Version of the system - if relevant | ||||
      |
Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
      |
Σ | 1..1 | string | Representation defined by the system | ||||
      |
Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
     |
Σ | 0..1 | string | Plain text representation of the concept | ||||
    |
S | 1..1 | positiveInt | Ranking of the diagnosis (for each role type) | ||||
   |
SΣ | 0..1 | BackboneElement | The list of diagnosis relevant to this encounter | ||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations | |||||
    |
?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
    |
Σ | 1..1 | Reference(Condition | Procedure) | The diagnosis or procedure relevant to the encounter | ||||
    |
0..1 | CodeableConcept | Role that this diagnosis has within the encounter (e.g. admission, billing, discharge …) Binding: DiagnosisRole (preferred): The type of diagnosis this condition represents. Fixed Value: As shown | |||||
     |
0..0 | string | Unique id for inter-element referencing | |||||
     |
0..0 | Extension | Additional content defined by implementations | |||||
     |
1..1 | Coding | Code defined by a terminology system Fixed Value: (complex) | |||||
      |
0..0 | string | Unique id for inter-element referencing | |||||
      |
0..0 | Extension | Additional content defined by implementations | |||||
      |
1..1 | uri | Identity of the terminology system Fixed Value: http://terminology.hl7.org/CodeSystem/diagnosis-role | |||||
      |
0..0 | string | Version of the system - if relevant | |||||
      |
1..1 | code | Symbol in syntax defined by the system Fixed Value: CC | |||||
      |
1..1 | string | Representation defined by the system Fixed Value: Chief complaint | |||||
      |
0..0 | boolean | If this coding was chosen directly by the user | |||||
     |
0..0 | string | Plain text representation of the concept | |||||
    |
0..1 | positiveInt | Ranking of the diagnosis (for each role type) | |||||
  |
S | 0..1 | BackboneElement | Details about the admission to a healthcare service | ||||
   |
0..1 | string | Unique id for inter-element referencing | |||||
   |
0..* | Extension | Extension Slice: Unordered, Open by value:url | |||||
    |
S | 0..1 | CodeableConcept | An extension to record how a patient was admitted to hospital URL: https://fhir.hl7.org.uk/StructureDefinition/Extension-UKCore-AdmissionMethod Binding: UK Core Admission Method (extensible): The method by which a patient was admitted to hospital | ||||
    |
S | 0..1 | (Complex) | Medically Safe for Discharge URL: https://fhir.interweavedigital.nhs.uk/R4/StructureDefinition/Extension-Interweave-MedicallySafeForDischarge | ||||
   |
?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
   |
0..1 | Identifier | Pre-admission identifier | |||||
   |
0..1 | Reference(Location | Organization) | The location from which the patient came before admission. Useful to provide if possible, in particular to reference a 'site' if transfered from another institution. | |||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
    |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    |
Σ | 0..1 | uri | Type the reference refers to (e.g. "Patient") Binding: ResourceType (extensible): Aa resource (or, for logical models, the URI of the logical model). | ||||
    |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
    |
Σ | 1..1 | string | Description of the referenced resource | ||||
   |
S | 0..1 | CodeableConcept | From where patient was admitted (physician referral, transfer) Binding: InterweaveAdmissionSource (required) | ||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
    |
Σ | 0..* | Coding | Code defined by a terminology system | ||||
     |
0..1 | string | Unique id for inter-element referencing | |||||
     |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
     |
Σ | 1..1 | uri | Identity of the terminology system | ||||
     |
Σ | 0..1 | string | Version of the system - if relevant | ||||
     |
Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
     |
Σ | 1..1 | string | Representation defined by the system | ||||
     |
Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
    |
Σ | 0..1 | string | Plain text representation of the concept | ||||
   |
0..1 | CodeableConcept | The type of hospital re-admission that has occurred (if any). If the value is absent, then this is not identified as a readmission Binding: hl7VS-re-admissionIndicator (example): The reason for re-admission of this hospitalization encounter. | |||||
   |
0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing Binding: Diet (example): Medical, cultural or ethical food preferences to help with catering requirements. | |||||
   |
0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing Binding: SpecialCourtesy (preferred): Special courtesies. | |||||
   |
0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing Binding: SpecialArrangements (preferred): Special arrangements. | |||||
   |
S | 0..1 | Reference(Location | Organization) | Location to which the patient is discharged. Important to provide if known to support discharge planning, and/or to reference a 'site' if transfered to another institution. | ||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
    |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    |
Σ | 0..1 | uri | Type the reference refers to (e.g. "Patient") Binding: ResourceType (extensible): Aa resource (or, for logical models, the URI of the logical model). | ||||
    |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
    |
Σ | 1..1 | string | Description of the referenced resource | ||||
   |
S | 0..1 | CodeableConcept | Category or kind of location after discharge Binding: InterweaveDischargeDestination (required) | ||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
    |
Σ | 0..* | Coding | Code defined by a terminology system | ||||
     |
0..1 | string | Unique id for inter-element referencing | |||||
     |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
     |
Σ | 1..1 | uri | Identity of the terminology system | ||||
     |
Σ | 0..1 | string | Version of the system - if relevant | ||||
     |
Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
     |
Σ | 1..1 | string | Representation defined by the system | ||||
     |
Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
    |
Σ | 0..1 | string | Plain text representation of the concept | ||||
  |
S | 0..* | BackboneElement | Location the encounter takes place (at Ward level) | ||||
   |
0..1 | string | Unique id for inter-element referencing | |||||
   |
0..* | Extension | Additional content defined by implementations | |||||
   |
?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
   |
S | 1..1 | Reference(Location) | Location the encounter takes place | ||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
    |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    |
Σ | 0..1 | uri | Type the reference refers to (e.g. "Patient") Binding: ResourceType (extensible): Aa resource (or, for logical models, the URI of the logical model). | ||||
    |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
    |
Σ | 1..1 | string | Description of the referenced resource | ||||
   |
S | 1..1 | code | planned | active | reserved | completed Binding: EncounterLocationStatus (required): The status of the location. | ||||
   |
0..1 | CodeableConcept | The physical type of the location (usually the level in the location hierachy - bed room ward etc.) Binding: UK Core Encounter Location Type (preferred): A set of codes that define the physical type of location where an encounter takes place. | |||||
   |
S | 1..1 | Period | Time period during which the patient was present at the location | ||||
  |
0..1 | Reference(Organization) | DISCOURAGED: This is instead covered via the provenance tags | |||||
  |
0..1 | Reference(InterweaveEncounterGrouping) | Another Encounter this encounter is part of | |||||
   |
0..1 | string | Unique id for inter-element referencing | |||||
   |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
   |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
   |
Σ | 0..1 | uri | Type the reference refers to (e.g. "Patient") Binding: ResourceType (extensible): Aa resource (or, for logical models, the URI of the logical model). | ||||
   |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
   |
Σ | 0..1 | string | If relevant, description of the referenced resource | ||||
 Documentation for this format Documentation for this format | ||||||||
| Path | Conformance | ValueSet / Code | URI | |||
| Encounter.meta.security | extensible | All Security Labelshttp://hl7.org/fhir/ValueSet/security-labelsfrom the FHIR Standard | ||||
| Encounter.meta.tag | example | CommonTagshttp://hl7.org/fhir/ValueSet/common-tagsfrom the FHIR Standard | ||||
| Encounter.meta.tag:Source | example | CommonTagshttp://hl7.org/fhir/ValueSet/common-tagsfrom the FHIR Standard | ||||
| Encounter.meta.tag:Provenance | example | CommonTagshttp://hl7.org/fhir/ValueSet/common-tagsfrom the FHIR Standard | ||||
| Encounter.language | preferred | CommonLanguages
http://hl7.org/fhir/ValueSet/languagesfrom the FHIR Standard | ||||
| Encounter.identifier.use | required | IdentifierUsehttp://hl7.org/fhir/ValueSet/identifier-use|4.0.1from the FHIR Standard | ||||
| Encounter.identifier.type | extensible | Identifier Type Codeshttp://hl7.org/fhir/ValueSet/identifier-typefrom the FHIR Standard | ||||
| Encounter.identifier:localIdentifier.use | required | IdentifierUsehttp://hl7.org/fhir/ValueSet/identifier-use|4.0.1from the FHIR Standard | ||||
| Encounter.identifier:localIdentifier.type | extensible | Identifier Type Codeshttp://hl7.org/fhir/ValueSet/identifier-typefrom the FHIR Standard | ||||
| Encounter.status | required | EncounterStatushttp://hl7.org/fhir/ValueSet/encounter-status|4.0.1from the FHIR Standard | ||||
| Encounter.statusHistory.status | required | EncounterStatushttp://hl7.org/fhir/ValueSet/encounter-status|4.0.1from the FHIR Standard | ||||
| Encounter.class | required | InterweaveEncounterClasshttps://fhir.interweavedigital.nhs.uk/R4/ValueSet/Interweave-EncounterClassfrom this IG | ||||
| Encounter.classHistory.class | extensible | ActEncounterCodehttp://terminology.hl7.org/ValueSet/v3-ActEncounterCode | ||||
| Encounter.type | required | UKCoreEncounterTypehttps://fhir.hl7.org.uk/ValueSet/UKCore-EncounterTypefrom this IG | ||||
| Encounter.serviceType | preferred | UKCoreCareSettingTypehttps://fhir.hl7.org.uk/ValueSet/UKCore-CareSettingTypefrom this IG | ||||
| Encounter.priority | required | InterweaveEncounterPriorityhttps://fhir.interweavedigital.nhs.uk/R4/ValueSet/Interweave-EncounterPriorityfrom this IG | ||||
| Encounter.subject.type | extensible | ResourceTypehttp://hl7.org/fhir/ValueSet/resource-typesfrom the FHIR Standard | ||||
| Encounter.basedOn.type | extensible | ResourceTypehttp://hl7.org/fhir/ValueSet/resource-typesfrom the FHIR Standard | ||||
| Encounter.participant.type | required | ParticipantTypehttp://hl7.org/fhir/ValueSet/encounter-participant-typefrom the FHIR Standard | ||||
| Encounter.participant.individual.type | extensible | ResourceTypehttp://hl7.org/fhir/ValueSet/resource-typesfrom the FHIR Standard | ||||
| Encounter.appointment.type | extensible | ResourceTypehttp://hl7.org/fhir/ValueSet/resource-typesfrom the FHIR Standard | ||||
| Encounter.reasonCode | preferred | EncounterReasonCodeshttp://hl7.org/fhir/ValueSet/encounter-reasonfrom the FHIR Standard | ||||
| Encounter.diagnosis.condition.type | extensible | ResourceTypehttp://hl7.org/fhir/ValueSet/resource-typesfrom the FHIR Standard | ||||
| Encounter.diagnosis.use | required | DiagnosisRolehttp://hl7.org/fhir/ValueSet/diagnosis-rolefrom the FHIR Standard | ||||
| Encounter.diagnosis:chiefComplaint.use | preferred | Fixed Value: CC("Chief complaint")http://hl7.org/fhir/ValueSet/diagnosis-rolefrom the FHIR Standard | ||||
| Encounter.hospitalization.origin.type | extensible | ResourceTypehttp://hl7.org/fhir/ValueSet/resource-typesfrom the FHIR Standard | ||||
| Encounter.hospitalization.admitSource | required | InterweaveAdmissionSourcehttps://fhir.interweavedigital.nhs.uk/R4/ValueSet/Interweave-AdmissionSourcefrom this IG | ||||
| Encounter.hospitalization.reAdmission | example | Hl7VSReAdmissionIndicatorhttp://terminology.hl7.org/ValueSet/v2-0092 | ||||
| Encounter.hospitalization.dietPreference | example | Diethttp://hl7.org/fhir/ValueSet/encounter-dietfrom the FHIR Standard | ||||
| Encounter.hospitalization.specialCourtesy | preferred | SpecialCourtesyhttp://hl7.org/fhir/ValueSet/encounter-special-courtesyfrom the FHIR Standard | ||||
| Encounter.hospitalization.specialArrangement | preferred | SpecialArrangementshttp://hl7.org/fhir/ValueSet/encounter-special-arrangementsfrom the FHIR Standard | ||||
| Encounter.hospitalization.destination.type | extensible | ResourceTypehttp://hl7.org/fhir/ValueSet/resource-typesfrom the FHIR Standard | ||||
| Encounter.hospitalization.dischargeDisposition | required | InterweaveDischargeDestinationhttps://fhir.interweavedigital.nhs.uk/R4/ValueSet/Interweave-DischargeDestinationfrom this IG | ||||
| Encounter.location.location.type | extensible | ResourceTypehttp://hl7.org/fhir/ValueSet/resource-typesfrom the FHIR Standard | ||||
| Encounter.location.status | required | EncounterLocationStatushttp://hl7.org/fhir/ValueSet/encounter-location-status|4.0.1from the FHIR Standard | ||||
| Encounter.location.physicalType | preferred | UKCoreEncounterLocationTypehttps://fhir.hl7.org.uk/ValueSet/UKCore-EncounterLocationTypefrom this IG | ||||
| Encounter.partOf.type | extensible | ResourceTypehttp://hl7.org/fhir/ValueSet/resource-typesfrom the FHIR Standard |
| Id | Grade | Path(s) | Details | Requirements |
| dom-2 | error | Encounter | If the resource is contained in another resource, it SHALL NOT contain nested Resources : contained.contained.empty() | |
| dom-3 | error | Encounter | If the resource is contained in another resource, it SHALL be referred to from elsewhere in the resource or SHALL refer to the containing resource : contained.where((('#'+id in (%resource.descendants().reference | %resource.descendants().as(canonical) | %resource.descendants().as(uri) | %resource.descendants().as(url))) or descendants().where(reference = '#').exists() or descendants().where(as(canonical) = '#').exists() or descendants().where(as(canonical) = '#').exists()).not()).trace('unmatched', id).empty() | |
| dom-4 | error | Encounter | If a resource is contained in another resource, it SHALL NOT have a meta.versionId or a meta.lastUpdated : contained.meta.versionId.empty() and contained.meta.lastUpdated.empty() | |
| dom-5 | error | Encounter | If a resource is contained in another resource, it SHALL NOT have a security label : contained.meta.security.empty() | |
| dom-6 | best practice | Encounter | A resource should have narrative for robust management : text.`div`.exists() | |
| ele-1 | error | **ALL** elements | All FHIR elements must have a @value or children : hasValue() or (children().count() > id.count()) | |
| ext-1 | error | **ALL** extensions | Must have either extensions or value[x], not both : extension.exists() != value.exists() |
This structure is derived from UKCoreEncounter
Summary
Mandatory: 13 elements(46 nested mandatory elements)
Must-Support: 40 elements
Fixed: 4 elements
Prohibited: 8 elements
Structures
This structure refers to these other structures:
Extensions
This structure refers to these extensions:
Slices
This structure defines the following Slices:
Differential View
This structure is derived from UKCoreEncounter
| Name | Flags | Card. | Type | Description & Constraints |
|---|---|---|---|---|
 |
UKCoreEncounter | |||
  |
S | 0..1 | id | Logical id of this artifact |
  |
||||
   |
0..0 | |||
   |
S | 0..1 | id | Version specific identifier |
   |
S | 0..1 | instant | MANDATORY except in Contained Resources. When the resource version last changed. |
   |
S | 0..* | canonical(StructureDefinition) | Profiles this resource claims to conform to. Should list (i) this profile (ii) base profile for this resource. |
   |
0..* | Coding | DISCOURAGED - may not be honoured by Data Consumers | |
   |
0..* | Coding | Tags applied to this resource Slice: Unordered, Open by value:system | |
    |
S | 0..1 | Coding | MANDATORY except in Contained Resources. The Data Provider Id (and display text) of the system supplying the data |
     |
0..0 | |||
     |
1..1 | uri | Identity of the terminology system Fixed Value: https://fhir.interweavedigital.nhs.uk/Source | |
     |
0..0 | |||
     |
S | 1..1 | code | The Data Provider Id of the system supplying the data |
     |
S | 1..1 | string | Name of the system supplying the data |
    |
S | 0..1 | Coding | MANDATORY except in Contained Resources. The ODS Code (and display text) of the organisation responsible for the data |
     |
0..0 | |||
     |
1..1 | uri | Identity of the terminology system Fixed Value: https://fhir.interweavedigital.nhs.uk/Provenance | |
     |
0..0 | |||
     |
S | 1..1 | code | The ODS Code of the organisation responsible for the data |
     |
S | 1..1 | string | Name of the organisation supplying the data |
  |
0..1 | uri | DISCOURAGED - may not be honoured by Data Consumers | |
  |
0..1 | code | English is assumed (not currently a multi-lingual implementation) | |
  |
0..1 | Narrative | DISCOURAGED - the preferred approach is to offer structured data fields which a Data Consumer can then render and present in a manner most suited to its users | |
  |
Content/Rules for all slices | |||
   |
S | 0..1 | ExtensionUKCoreEmergencyCareDischargeStatus | An extension used indicate the status of a patient on discharge from an Emergency Care Department |
   |
S | 0..1 | CodeableConcept | Discharge destination of patients which have attended ED. URL: https://fhir.interweavedigital.nhs.uk/R4/StructureDefinition/Extension-Interweave-EDDischargeDestination Binding: InterweaveEDDischargeDestination (preferred) |
  |
0..* | Identifier | Identifier(s) by which this encounter is known. Slice: Unordered, Open by value:system | |
   |
Content/Rules for all slices | |||
    |
0..1 | Reference(InterweaveOrganization) | Organization that issued id (may be just text) | |
   |
S | 0..1 | Identifier | Identifier(s) by which this encounter is known. |
    |
S | 1..1 | uri | The namespace for the identifier value Fixed Value: https://fhir.interweavedigital.nhs.uk/Id/local-encounter-identifier |
    |
S | 1..1 | string | The Local encounter Identifier. Please prefix with ODS code plus period (XXX.) to ensure unique |
    |
0..0 | |||
  |
1..1 | code | arrived | triaged | in-progress | onleave | finished | cancelled | entered-in-error | unknown (Note: 'planned' is also possible, but normally represented instead as an Appointment) | |
  |
S | 0..* | BackboneElement | List of past encounter statuses |
  |
1..1 | Coding | Classification of the encounter. EXTENSIBLE on request, eg to cover other care settings Binding: InterweaveEncounterClass (required) | |
   |
1..1 | uri | Identity of the terminology system | |
   |
1..1 | code | Symbol in syntax defined by the system | |
   |
1..1 | string | Representation defined by the system | |
  |
0..0 | |||
  |
S | 0..1 | CodeableConcept | Specific type of encounter Binding: UK Core Encounter Type (required) |
   |
||||
    |
1..1 | uri | Identity of the terminology system | |
    |
1..1 | code | Symbol in syntax defined by the system | |
    |
1..1 | string | Representation defined by the system | |
  |
S | 0..1 | CodeableConcept | Specific type of service |
   |
||||
    |
1..1 | uri | Identity of the terminology system | |
    |
1..1 | code | Symbol in syntax defined by the system | |
    |
1..1 | string | Representation defined by the system | |
  |
S | 0..1 | CodeableConcept | Indicates the urgency of the encounter Binding: InterweaveEncounterPriority (required) |
   |
||||
    |
1..1 | uri | Identity of the terminology system | |
    |
1..1 | code | Symbol in syntax defined by the system | |
    |
1..1 | string | Representation defined by the system | |
  |
1..1 | Reference(InterweavePatient) | The patient (NOT group) present at the encounter | |
   |
1..1 | string | Reference to a resource (could be Contained) | |
   |
0..1 | Identifier | If relevant could include an id | |
   |
1..1 | string | Description of the referenced resource | |
  |
||||
   |
1..1 | string | Reference to a resource (could be Contained) | |
   |
0..1 | Identifier | If relevant could include an id | |
   |
0..1 | string | If relevant, description of the referenced resource | |
  |
1..* | BackboneElement | The list of people responsible for providing the service. | |
   |
S | 1..1 | CodeableConcept | Role of participant in encounter Binding: ParticipantType (required) |
    |
||||
     |
1..1 | uri | Identity of the terminology system | |
     |
1..1 | code | Symbol in syntax defined by the system | |
     |
1..1 | string | Representation defined by the system | |
   |
S | 1..1 | Reference(InterweavePractitioner) | Persons involved in the encounter other than the patient |
    |
1..1 | string | Reference to a resource (could be Contained) | |
    |
0..1 | Identifier | If relevant could include an id | |
    |
1..1 | string | Description of the referenced resource | |
  |
S | 0..1 | Reference(Appointment) | The appointment that scheduled this encounter |
   |
1..1 | string | Reference to a resource (could be Contained) | |
   |
0..1 | Identifier | If relevant could include an id | |
   |
0..1 | string | If relevant, description of the referenced resource | |
  |
S | 1..1 | Period | The start and end time of the encounter |
   |
S | 1..1 | dateTime | Starting time with inclusive boundary |
   |
S | 0..1 | dateTime | End time with inclusive boundary, if not ongoing |
  |
0..1 | Duration | Quantity of time the encounter lasted (less time absent). Please use minutes. | |
  |
||||
   |
||||
    |
1..1 | uri | Identity of the terminology system | |
    |
1..1 | code | Symbol in syntax defined by the system | |
    |
1..1 | string | Representation defined by the system | |
  |
S | 0..* | BackboneElement | The list of diagnosis relevant to this encounter Slice: Unordered, Open by value:use |
   |
Content/Rules for all slices | |||
    |
S | 1..1 | Reference(Condition | Procedure) | The diagnosis or procedure relevant to the encounter |
     |
1..1 | string | Reference to a resource (could be Contained) | |
     |
0..1 | Identifier | If relevant could include an id | |
     |
0..1 | string | If relevant, description of the referenced resource | |
    |
S | 1..1 | CodeableConcept | Role that this diagnosis has within the encounter (e.g. admission, billing, discharge …) Binding: DiagnosisRole (required) |
     |
||||
      |
1..1 | uri | Identity of the terminology system | |
      |
1..1 | code | Symbol in syntax defined by the system | |
      |
1..1 | string | Representation defined by the system | |
    |
S | 1..1 | positiveInt | Ranking of the diagnosis (for each role type) |
   |
S | 0..1 | BackboneElement | The list of diagnosis relevant to this encounter |
    |
0..1 | CodeableConcept | Role that this diagnosis has within the encounter (e.g. admission, billing, discharge …) Fixed Value: As shown | |
     |
1..1 | Coding | Code defined by a terminology system Fixed Value: (complex) | |
      |
1..1 | uri | Identity of the terminology system Fixed Value: http://terminology.hl7.org/CodeSystem/diagnosis-role | |
      |
1..1 | code | Symbol in syntax defined by the system Fixed Value: CC | |
      |
1..1 | string | Representation defined by the system Fixed Value: Chief complaint | |
  |
0..0 | |||
  |
S | 0..1 | BackboneElement | Details about the admission to a healthcare service |
   |
Content/Rules for all slices | |||
    |
S | 0..1 | ExtensionUKCoreAdmissionMethod | An extension to record how a patient was admitted to hospital |
    |
S | 0..1 | (Complex) | Medically Safe for Discharge URL: https://fhir.interweavedigital.nhs.uk/R4/StructureDefinition/Extension-Interweave-MedicallySafeForDischarge |
   |
0..1 | Reference(Location | Organization) | The location from which the patient came before admission. Useful to provide if possible, in particular to reference a 'site' if transfered from another institution. | |
    |
1..1 | string | Reference to a resource (could be Contained) | |
    |
0..1 | Identifier | If relevant could include an id | |
    |
1..1 | string | Description of the referenced resource | |
   |
S | 0..1 | CodeableConcept | From where patient was admitted (physician referral, transfer) Binding: InterweaveAdmissionSource (required) |
    |
||||
     |
1..1 | uri | Identity of the terminology system | |
     |
1..1 | code | Symbol in syntax defined by the system | |
     |
1..1 | string | Representation defined by the system | |
   |
0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing | |
   |
0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing | |
   |
0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing | |
   |
S | 0..1 | Reference(Location | Organization) | Location to which the patient is discharged. Important to provide if known to support discharge planning, and/or to reference a 'site' if transfered to another institution. |
    |
1..1 | string | Reference to a resource (could be Contained) | |
    |
0..1 | Identifier | If relevant could include an id | |
    |
1..1 | string | Description of the referenced resource | |
   |
S | 0..1 | CodeableConcept | Category or kind of location after discharge Binding: InterweaveDischargeDestination (required) |
    |
||||
     |
1..1 | uri | Identity of the terminology system | |
     |
1..1 | code | Symbol in syntax defined by the system | |
     |
1..1 | string | Representation defined by the system | |
  |
S | 0..* | BackboneElement | Location the encounter takes place (at Ward level) |
   |
S | 1..1 | Reference(Location) | Location the encounter takes place |
    |
1..1 | string | Reference to a resource (could be Contained) | |
    |
0..1 | Identifier | If relevant could include an id | |
    |
1..1 | string | Description of the referenced resource | |
   |
S | 1..1 | code | planned | active | reserved | completed |
   |
S | 1..1 | Period | Time period during which the patient was present at the location |
  |
0..1 | Reference(Organization) | DISCOURAGED: This is instead covered via the provenance tags | |
  |
0..1 | Reference(InterweaveEncounterGrouping) | Another Encounter this encounter is part of | |
   |
1..1 | string | Reference to a resource (could be Contained) | |
   |
0..1 | Identifier | If relevant could include an id | |
   |
0..1 | string | If relevant, description of the referenced resource | |
 Documentation for this format Documentation for this format | ||||
| Path | Conformance | ValueSet | URI |
| Encounter.class | required | InterweaveEncounterClasshttps://fhir.interweavedigital.nhs.uk/R4/ValueSet/Interweave-EncounterClassfrom this IG | |
| Encounter.type | required | UKCoreEncounterTypehttps://fhir.hl7.org.uk/ValueSet/UKCore-EncounterTypefrom this IG | |
| Encounter.priority | required | InterweaveEncounterPriorityhttps://fhir.interweavedigital.nhs.uk/R4/ValueSet/Interweave-EncounterPriorityfrom this IG | |
| Encounter.participant.type | required | ParticipantTypehttp://hl7.org/fhir/ValueSet/encounter-participant-typefrom the FHIR Standard | |
| Encounter.diagnosis.use | required | DiagnosisRolehttp://hl7.org/fhir/ValueSet/diagnosis-rolefrom the FHIR Standard | |
| Encounter.hospitalization.admitSource | required | InterweaveAdmissionSourcehttps://fhir.interweavedigital.nhs.uk/R4/ValueSet/Interweave-AdmissionSourcefrom this IG | |
| Encounter.hospitalization.dischargeDisposition | required | InterweaveDischargeDestinationhttps://fhir.interweavedigital.nhs.uk/R4/ValueSet/Interweave-DischargeDestinationfrom this IG |
Key Elements View
| Name | Flags | Card. | Type | Description & Constraints | ||||
|---|---|---|---|---|---|---|---|---|
 |
0..* | UKCoreEncounter | An interaction during which services are provided to the patient | |||||
  |
SΣ | 0..1 | id | Logical id of this artifact | ||||
  |
Σ | 0..1 | Meta | Metadata about the resource | ||||
   |
SΣ | 0..1 | id | Version specific identifier | ||||
   |
SΣ | 0..1 | instant | MANDATORY except in Contained Resources. When the resource version last changed. | ||||
   |
SΣ | 0..* | canonical(StructureDefinition) | Profiles this resource claims to conform to. Should list (i) this profile (ii) base profile for this resource. | ||||
   |
Σ | 0..* | Coding | DISCOURAGED - may not be honoured by Data Consumers Binding: All Security Labels (extensible): Security Labels from the Healthcare Privacy and Security Classification System. | ||||
   |
Σ | 0..* | Coding | Tags applied to this resource Slice: Unordered, Open by value:system Binding: CommonTags (example): Codes that represent various types of tags, commonly workflow-related; e.g. "Needs review by Dr. Jones". | ||||
    |
SΣ | 0..1 | Coding | MANDATORY except in Contained Resources. The Data Provider Id (and display text) of the system supplying the data Binding: CommonTags (example): Codes that represent various types of tags, commonly workflow-related; e.g. "Needs review by Dr. Jones". | ||||
     |
Σ | 1..1 | uri | Identity of the terminology system Fixed Value: https://fhir.interweavedigital.nhs.uk/Source | ||||
     |
SΣ | 1..1 | code | The Data Provider Id of the system supplying the data | ||||
     |
SΣ | 1..1 | string | Name of the system supplying the data | ||||
    |
SΣ | 0..1 | Coding | MANDATORY except in Contained Resources. The ODS Code (and display text) of the organisation responsible for the data Binding: CommonTags (example): Codes that represent various types of tags, commonly workflow-related; e.g. "Needs review by Dr. Jones". | ||||
     |
Σ | 1..1 | uri | Identity of the terminology system Fixed Value: https://fhir.interweavedigital.nhs.uk/Provenance | ||||
     |
SΣ | 1..1 | code | The ODS Code of the organisation responsible for the data | ||||
     |
SΣ | 1..1 | string | Name of the organisation supplying the data | ||||
  |
?!Σ | 0..1 | uri | DISCOURAGED - may not be honoured by Data Consumers | ||||
  |
0..1 | code | English is assumed (not currently a multi-lingual implementation) Binding: CommonLanguages (preferred): A human language.
| |||||
  |
0..1 | Narrative | DISCOURAGED - the preferred approach is to offer structured data fields which a Data Consumer can then render and present in a manner most suited to its users | |||||
  |
Content/Rules for all slices | |||||||
   |
0..1 | CodeableConcept | An extension to support the method of discharge from a hospital. URL: https://fhir.hl7.org.uk/StructureDefinition/Extension-UKCore-DischargeMethod Binding: UK Core Discharge Method (extensible): The method by which a patient was discharged from hospital | |||||
   |
S | 0..1 | CodeableConcept | An extension used indicate the status of a patient on discharge from an Emergency Care Department URL: https://fhir.hl7.org.uk/StructureDefinition/Extension-UKCore-EmergencyCareDischargeStatus Binding: UK Core Emergency Care Discharge Status (preferred): The status of a patient on discharge from an Emergency Care Department | ||||
   |
0..* | (Complex) | Information relating to a patient's legal status on admission or discharge. URL: https://fhir.hl7.org.uk/StructureDefinition/Extension-UKCore-LegalStatus | |||||
   |
0..1 | CodeableConcept | An extension to support the outcome of an Outpatient attendance. URL: https://fhir.hl7.org.uk/StructureDefinition/Extension-UKCore-OutcomeOfAttendance Binding: UK Core Outcome Of Attendance (extensible): The outcome of an outpatient attendance | |||||
   |
S | 0..1 | CodeableConcept | Discharge destination of patients which have attended ED. URL: https://fhir.interweavedigital.nhs.uk/R4/StructureDefinition/Extension-Interweave-EDDischargeDestination Binding: InterweaveEDDischargeDestination (preferred) | ||||
  |
?! | 0..* | Extension | Extensions that cannot be ignored | ||||
  |
SΣ | 0..* | Identifier | Identifier(s) by which this encounter is known. Slice: Unordered, Open by value:system | ||||
   |
Content/Rules for all slices | |||||||
    |
?!Σ | 0..1 | code | usual | official | temp | secondary | old (If known) Binding: IdentifierUse (required): Identifies the purpose for this identifier, if known . | ||||
    |
Σ | 0..1 | Reference(InterweaveOrganization) | Organization that issued id (may be just text) | ||||
   |
SΣ | 0..1 | Identifier | Identifier(s) by which this encounter is known. | ||||
    |
?!Σ | 0..1 | code | usual | official | temp | secondary | old (If known) Binding: IdentifierUse (required): Identifies the purpose for this identifier, if known . | ||||
    |
SΣ | 1..1 | uri | The namespace for the identifier value Fixed Value: https://fhir.interweavedigital.nhs.uk/Id/local-encounter-identifier | ||||
    |
SΣ | 1..1 | string | The Local encounter Identifier. Please prefix with ODS code plus period (XXX.) to ensure unique Example General: 123456 | ||||
  |
?!SΣ | 1..1 | code | arrived | triaged | in-progress | onleave | finished | cancelled | entered-in-error | unknown (Note: 'planned' is also possible, but normally represented instead as an Appointment) Binding: EncounterStatus (required): Current state of the encounter. | ||||
  |
S | 0..* | BackboneElement | List of past encounter statuses | ||||
   |
?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
   |
1..1 | code | planned | arrived | triaged | in-progress | onleave | finished | cancelled + Binding: EncounterStatus (required): Current state of the encounter. | |||||
   |
1..1 | Period | The time that the episode was in the specified status | |||||
  |
SΣ | 1..1 | Coding | Classification of the encounter. EXTENSIBLE on request, eg to cover other care settings Binding: InterweaveEncounterClass (required) | ||||
   |
Σ | 1..1 | uri | Identity of the terminology system | ||||
   |
Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
   |
Σ | 1..1 | string | Representation defined by the system | ||||
  |
SΣ | 0..1 | CodeableConcept | Specific type of encounter Binding: UK Core Encounter Type (required) | ||||
  |
SΣ | 0..1 | CodeableConcept | Specific type of service Binding: UK Core Care Setting Type (preferred): Any code from the SNOMED CT UK Refset with fully specified name 'Services simple reference set (foundation metadata concept)' with Refset Id 1127531000000102. | ||||
  |
S | 0..1 | CodeableConcept | Indicates the urgency of the encounter Binding: InterweaveEncounterPriority (required) | ||||
  |
SΣ | 1..1 | Reference(InterweavePatient) | The patient (NOT group) present at the encounter | ||||
   |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
   |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
   |
Σ | 1..1 | string | Description of the referenced resource | ||||
  |
SΣ | 1..* | BackboneElement | The list of people responsible for providing the service. | ||||
   |
?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
   |
SΣ | 1..1 | CodeableConcept | Role of participant in encounter Binding: ParticipantType (required) | ||||
   |
SΣ | 1..1 | Reference(InterweavePractitioner) | Persons involved in the encounter other than the patient | ||||
    |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
    |
Σ | 1..1 | string | Description of the referenced resource | ||||
  |
SΣ | 0..1 | Reference(Appointment) | The appointment that scheduled this encounter | ||||
   |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
   |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
   |
Σ | 0..1 | string | If relevant, description of the referenced resource | ||||
  |
S | 1..1 | Period | The start and end time of the encounter | ||||
   |
SΣC | 1..1 | dateTime | Starting time with inclusive boundary | ||||
   |
SΣC | 0..1 | dateTime | End time with inclusive boundary, if not ongoing | ||||
  |
0..1 | Duration | Quantity of time the encounter lasted (less time absent). Please use minutes. | |||||
  |
SΣ | 0..* | CodeableConcept | Reason the encounter takes place, expressed as a code. For admissions, this can be used for a coded admission diagnosis. Binding: EncounterReasonCodes (preferred): Reason why the encounter takes place. | ||||
  |
SΣ | 0..* | Reference(Condition | Procedure | Observation | ImmunizationRecommendation) | Reason the encounter takes place, expressed as a reference to a Condition, Procedure, Observation, or ImmunizationRecommendation. | ||||
  |
SΣ | 0..* | BackboneElement | The list of diagnosis relevant to this encounter Slice: Unordered, Open by value:use | ||||
   |
Content/Rules for all slices | |||||||
    |
?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
    |
SΣ | 1..1 | Reference(Condition | Procedure) | The diagnosis or procedure relevant to the encounter | ||||
     |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
     |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
     |
Σ | 0..1 | string | If relevant, description of the referenced resource | ||||
    |
S | 1..1 | CodeableConcept | Role that this diagnosis has within the encounter (e.g. admission, billing, discharge …) Binding: DiagnosisRole (required) | ||||
    |
S | 1..1 | positiveInt | Ranking of the diagnosis (for each role type) | ||||
   |
SΣ | 0..1 | BackboneElement | The list of diagnosis relevant to this encounter | ||||
    |
?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
    |
Σ | 1..1 | Reference(Condition | Procedure) | The diagnosis or procedure relevant to the encounter | ||||
    |
0..1 | CodeableConcept | Role that this diagnosis has within the encounter (e.g. admission, billing, discharge …) Binding: DiagnosisRole (preferred): The type of diagnosis this condition represents. Fixed Value: As shown | |||||
     |
0..0 | string | Unique id for inter-element referencing | |||||
     |
0..0 | Extension | Additional content defined by implementations | |||||
     |
1..1 | Coding | Code defined by a terminology system Fixed Value: (complex) | |||||
      |
0..0 | string | Unique id for inter-element referencing | |||||
      |
0..0 | Extension | Additional content defined by implementations | |||||
      |
1..1 | uri | Identity of the terminology system Fixed Value: http://terminology.hl7.org/CodeSystem/diagnosis-role | |||||
      |
0..0 | string | Version of the system - if relevant | |||||
      |
1..1 | code | Symbol in syntax defined by the system Fixed Value: CC | |||||
      |
1..1 | string | Representation defined by the system Fixed Value: Chief complaint | |||||
      |
0..0 | boolean | If this coding was chosen directly by the user | |||||
     |
0..0 | string | Plain text representation of the concept | |||||
  |
S | 0..1 | BackboneElement | Details about the admission to a healthcare service | ||||
   |
Content/Rules for all slices | |||||||
    |
S | 0..1 | CodeableConcept | An extension to record how a patient was admitted to hospital URL: https://fhir.hl7.org.uk/StructureDefinition/Extension-UKCore-AdmissionMethod Binding: UK Core Admission Method (extensible): The method by which a patient was admitted to hospital | ||||
    |
S | 0..1 | (Complex) | Medically Safe for Discharge URL: https://fhir.interweavedigital.nhs.uk/R4/StructureDefinition/Extension-Interweave-MedicallySafeForDischarge | ||||
   |
?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
   |
0..1 | Reference(Location | Organization) | The location from which the patient came before admission. Useful to provide if possible, in particular to reference a 'site' if transfered from another institution. | |||||
    |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
    |
Σ | 1..1 | string | Description of the referenced resource | ||||
   |
S | 0..1 | CodeableConcept | From where patient was admitted (physician referral, transfer) Binding: InterweaveAdmissionSource (required) | ||||
   |
0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing Binding: Diet (example): Medical, cultural or ethical food preferences to help with catering requirements. | |||||
   |
0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing Binding: SpecialCourtesy (preferred): Special courtesies. | |||||
   |
0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing Binding: SpecialArrangements (preferred): Special arrangements. | |||||
   |
S | 0..1 | Reference(Location | Organization) | Location to which the patient is discharged. Important to provide if known to support discharge planning, and/or to reference a 'site' if transfered to another institution. | ||||
    |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
    |
Σ | 1..1 | string | Description of the referenced resource | ||||
   |
S | 0..1 | CodeableConcept | Category or kind of location after discharge Binding: InterweaveDischargeDestination (required) | ||||
  |
S | 0..* | BackboneElement | Location the encounter takes place (at Ward level) | ||||
   |
?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
   |
S | 1..1 | Reference(Location) | Location the encounter takes place | ||||
    |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
    |
Σ | 1..1 | string | Description of the referenced resource | ||||
   |
S | 1..1 | code | planned | active | reserved | completed Binding: EncounterLocationStatus (required): The status of the location. | ||||
   |
S | 1..1 | Period | Time period during which the patient was present at the location | ||||
  |
0..1 | Reference(Organization) | DISCOURAGED: This is instead covered via the provenance tags | |||||
  |
0..1 | Reference(InterweaveEncounterGrouping) | Another Encounter this encounter is part of | |||||
   |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
   |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
   |
Σ | 0..1 | string | If relevant, description of the referenced resource | ||||
 Documentation for this format Documentation for this format | ||||||||
| Path | Conformance | ValueSet / Code | URI | |||
| Encounter.meta.security | extensible | All Security Labelshttp://hl7.org/fhir/ValueSet/security-labelsfrom the FHIR Standard | ||||
| Encounter.meta.tag | example | CommonTagshttp://hl7.org/fhir/ValueSet/common-tagsfrom the FHIR Standard | ||||
| Encounter.meta.tag:Source | example | CommonTagshttp://hl7.org/fhir/ValueSet/common-tagsfrom the FHIR Standard | ||||
| Encounter.meta.tag:Provenance | example | CommonTagshttp://hl7.org/fhir/ValueSet/common-tagsfrom the FHIR Standard | ||||
| Encounter.language | preferred | CommonLanguages
http://hl7.org/fhir/ValueSet/languagesfrom the FHIR Standard | ||||
| Encounter.identifier.use | required | IdentifierUsehttp://hl7.org/fhir/ValueSet/identifier-use|4.0.1from the FHIR Standard | ||||
| Encounter.identifier:localIdentifier.use | required | IdentifierUsehttp://hl7.org/fhir/ValueSet/identifier-use|4.0.1from the FHIR Standard | ||||
| Encounter.status | required | EncounterStatushttp://hl7.org/fhir/ValueSet/encounter-status|4.0.1from the FHIR Standard | ||||
| Encounter.statusHistory.status | required | EncounterStatushttp://hl7.org/fhir/ValueSet/encounter-status|4.0.1from the FHIR Standard | ||||
| Encounter.class | required | InterweaveEncounterClasshttps://fhir.interweavedigital.nhs.uk/R4/ValueSet/Interweave-EncounterClassfrom this IG | ||||
| Encounter.classHistory.class | extensible | ActEncounterCodehttp://terminology.hl7.org/ValueSet/v3-ActEncounterCode | ||||
| Encounter.type | required | UKCoreEncounterTypehttps://fhir.hl7.org.uk/ValueSet/UKCore-EncounterTypefrom this IG | ||||
| Encounter.serviceType | preferred | UKCoreCareSettingTypehttps://fhir.hl7.org.uk/ValueSet/UKCore-CareSettingTypefrom this IG | ||||
| Encounter.priority | required | InterweaveEncounterPriorityhttps://fhir.interweavedigital.nhs.uk/R4/ValueSet/Interweave-EncounterPriorityfrom this IG | ||||
| Encounter.participant.type | required | ParticipantTypehttp://hl7.org/fhir/ValueSet/encounter-participant-typefrom the FHIR Standard | ||||
| Encounter.reasonCode | preferred | EncounterReasonCodeshttp://hl7.org/fhir/ValueSet/encounter-reasonfrom the FHIR Standard | ||||
| Encounter.diagnosis.use | required | DiagnosisRolehttp://hl7.org/fhir/ValueSet/diagnosis-rolefrom the FHIR Standard | ||||
| Encounter.diagnosis:chiefComplaint.use | preferred | Fixed Value: CC("Chief complaint")http://hl7.org/fhir/ValueSet/diagnosis-rolefrom the FHIR Standard | ||||
| Encounter.hospitalization.admitSource | required | InterweaveAdmissionSourcehttps://fhir.interweavedigital.nhs.uk/R4/ValueSet/Interweave-AdmissionSourcefrom this IG | ||||
| Encounter.hospitalization.dietPreference | example | Diethttp://hl7.org/fhir/ValueSet/encounter-dietfrom the FHIR Standard | ||||
| Encounter.hospitalization.specialCourtesy | preferred | SpecialCourtesyhttp://hl7.org/fhir/ValueSet/encounter-special-courtesyfrom the FHIR Standard | ||||
| Encounter.hospitalization.specialArrangement | preferred | SpecialArrangementshttp://hl7.org/fhir/ValueSet/encounter-special-arrangementsfrom the FHIR Standard | ||||
| Encounter.hospitalization.dischargeDisposition | required | InterweaveDischargeDestinationhttps://fhir.interweavedigital.nhs.uk/R4/ValueSet/Interweave-DischargeDestinationfrom this IG | ||||
| Encounter.location.status | required | EncounterLocationStatushttp://hl7.org/fhir/ValueSet/encounter-location-status|4.0.1from the FHIR Standard |
| Id | Grade | Path(s) | Details | Requirements |
| dom-2 | error | Encounter | If the resource is contained in another resource, it SHALL NOT contain nested Resources : contained.contained.empty() | |
| dom-3 | error | Encounter | If the resource is contained in another resource, it SHALL be referred to from elsewhere in the resource or SHALL refer to the containing resource : contained.where((('#'+id in (%resource.descendants().reference | %resource.descendants().as(canonical) | %resource.descendants().as(uri) | %resource.descendants().as(url))) or descendants().where(reference = '#').exists() or descendants().where(as(canonical) = '#').exists() or descendants().where(as(canonical) = '#').exists()).not()).trace('unmatched', id).empty() | |
| dom-4 | error | Encounter | If a resource is contained in another resource, it SHALL NOT have a meta.versionId or a meta.lastUpdated : contained.meta.versionId.empty() and contained.meta.lastUpdated.empty() | |
| dom-5 | error | Encounter | If a resource is contained in another resource, it SHALL NOT have a security label : contained.meta.security.empty() | |
| dom-6 | best practice | Encounter | A resource should have narrative for robust management : text.`div`.exists() | |
| ele-1 | error | **ALL** elements | All FHIR elements must have a @value or children : hasValue() or (children().count() > id.count()) | |
| ext-1 | error | **ALL** extensions | Must have either extensions or value[x], not both : extension.exists() != value.exists() |
Snapshot View
| Name | Flags | Card. | Type | Description & Constraints | ||||
|---|---|---|---|---|---|---|---|---|
 |
0..* | UKCoreEncounter | An interaction during which services are provided to the patient | |||||
  |
SΣ | 0..1 | id | Logical id of this artifact | ||||
  |
Σ | 0..1 | Meta | Metadata about the resource | ||||
   |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
   |
SΣ | 0..1 | id | Version specific identifier | ||||
   |
SΣ | 0..1 | instant | MANDATORY except in Contained Resources. When the resource version last changed. | ||||
   |
Σ | 0..1 | uri | Identifies where the resource comes from | ||||
   |
SΣ | 0..* | canonical(StructureDefinition) | Profiles this resource claims to conform to. Should list (i) this profile (ii) base profile for this resource. | ||||
   |
Σ | 0..* | Coding | DISCOURAGED - may not be honoured by Data Consumers Binding: All Security Labels (extensible): Security Labels from the Healthcare Privacy and Security Classification System. | ||||
   |
Σ | 0..* | Coding | Tags applied to this resource Slice: Unordered, Open by value:system Binding: CommonTags (example): Codes that represent various types of tags, commonly workflow-related; e.g. "Needs review by Dr. Jones". | ||||
    |
SΣ | 0..1 | Coding | MANDATORY except in Contained Resources. The Data Provider Id (and display text) of the system supplying the data Binding: CommonTags (example): Codes that represent various types of tags, commonly workflow-related; e.g. "Needs review by Dr. Jones". | ||||
     |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
     |
Σ | 1..1 | uri | Identity of the terminology system Fixed Value: https://fhir.interweavedigital.nhs.uk/Source | ||||
     |
SΣ | 1..1 | code | The Data Provider Id of the system supplying the data | ||||
     |
SΣ | 1..1 | string | Name of the system supplying the data | ||||
     |
Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
    |
SΣ | 0..1 | Coding | MANDATORY except in Contained Resources. The ODS Code (and display text) of the organisation responsible for the data Binding: CommonTags (example): Codes that represent various types of tags, commonly workflow-related; e.g. "Needs review by Dr. Jones". | ||||
     |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
     |
Σ | 1..1 | uri | Identity of the terminology system Fixed Value: https://fhir.interweavedigital.nhs.uk/Provenance | ||||
     |
SΣ | 1..1 | code | The ODS Code of the organisation responsible for the data | ||||
     |
SΣ | 1..1 | string | Name of the organisation supplying the data | ||||
     |
Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
  |
?!Σ | 0..1 | uri | DISCOURAGED - may not be honoured by Data Consumers | ||||
  |
0..1 | code | English is assumed (not currently a multi-lingual implementation) Binding: CommonLanguages (preferred): A human language.
| |||||
  |
0..1 | Narrative | DISCOURAGED - the preferred approach is to offer structured data fields which a Data Consumer can then render and present in a manner most suited to its users | |||||
  |
0..* | Resource | Contained, inline Resources | |||||
  |
0..* | Extension | Extension Slice: Unordered, Open by value:url | |||||
   |
0..1 | CodeableConcept | An extension to support the method of discharge from a hospital. URL: https://fhir.hl7.org.uk/StructureDefinition/Extension-UKCore-DischargeMethod Binding: UK Core Discharge Method (extensible): The method by which a patient was discharged from hospital | |||||
   |
S | 0..1 | CodeableConcept | An extension used indicate the status of a patient on discharge from an Emergency Care Department URL: https://fhir.hl7.org.uk/StructureDefinition/Extension-UKCore-EmergencyCareDischargeStatus Binding: UK Core Emergency Care Discharge Status (preferred): The status of a patient on discharge from an Emergency Care Department | ||||
   |
0..* | (Complex) | Information relating to a patient's legal status on admission or discharge. URL: https://fhir.hl7.org.uk/StructureDefinition/Extension-UKCore-LegalStatus | |||||
   |
0..1 | CodeableConcept | An extension to support the outcome of an Outpatient attendance. URL: https://fhir.hl7.org.uk/StructureDefinition/Extension-UKCore-OutcomeOfAttendance Binding: UK Core Outcome Of Attendance (extensible): The outcome of an outpatient attendance | |||||
   |
S | 0..1 | CodeableConcept | Discharge destination of patients which have attended ED. URL: https://fhir.interweavedigital.nhs.uk/R4/StructureDefinition/Extension-Interweave-EDDischargeDestination Binding: InterweaveEDDischargeDestination (preferred) | ||||
  |
?! | 0..* | Extension | Extensions that cannot be ignored | ||||
  |
SΣ | 0..* | Identifier | Identifier(s) by which this encounter is known. Slice: Unordered, Open by value:system | ||||
   |
Content/Rules for all slices | |||||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
    |
?!Σ | 0..1 | code | usual | official | temp | secondary | old (If known) Binding: IdentifierUse (required): Identifies the purpose for this identifier, if known . | ||||
    |
Σ | 0..1 | CodeableConcept | Description of identifier Binding: Identifier Type Codes (extensible): A coded type for an identifier that can be used to determine which identifier to use for a specific purpose. | ||||
    |
Σ | 0..1 | uri | The namespace for the identifier value Example General: http://www.acme.com/identifiers/patient | ||||
    |
Σ | 0..1 | string | The value that is unique Example General: 123456 | ||||
    |
Σ | 0..1 | Period | Time period when id is/was valid for use | ||||
    |
Σ | 0..1 | Reference(InterweaveOrganization) | Organization that issued id (may be just text) | ||||
   |
SΣ | 0..1 | Identifier | Identifier(s) by which this encounter is known. | ||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
    |
?!Σ | 0..1 | code | usual | official | temp | secondary | old (If known) Binding: IdentifierUse (required): Identifies the purpose for this identifier, if known . | ||||
    |
Σ | 0..1 | CodeableConcept | Description of identifier Binding: Identifier Type Codes (extensible): A coded type for an identifier that can be used to determine which identifier to use for a specific purpose. | ||||
    |
SΣ | 1..1 | uri | The namespace for the identifier value Fixed Value: https://fhir.interweavedigital.nhs.uk/Id/local-encounter-identifier | ||||
    |
SΣ | 1..1 | string | The Local encounter Identifier. Please prefix with ODS code plus period (XXX.) to ensure unique Example General: 123456 | ||||
    |
Σ | 0..1 | Reference(Organization) | Organization that issued id (may be just text) | ||||
  |
?!SΣ | 1..1 | code | arrived | triaged | in-progress | onleave | finished | cancelled | entered-in-error | unknown (Note: 'planned' is also possible, but normally represented instead as an Appointment) Binding: EncounterStatus (required): Current state of the encounter. | ||||
  |
S | 0..* | BackboneElement | List of past encounter statuses | ||||
   |
0..1 | string | Unique id for inter-element referencing | |||||
   |
0..* | Extension | Additional content defined by implementations | |||||
   |
?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
   |
1..1 | code | planned | arrived | triaged | in-progress | onleave | finished | cancelled + Binding: EncounterStatus (required): Current state of the encounter. | |||||
   |
1..1 | Period | The time that the episode was in the specified status | |||||
  |
SΣ | 1..1 | Coding | Classification of the encounter. EXTENSIBLE on request, eg to cover other care settings Binding: InterweaveEncounterClass (required) | ||||
   |
0..1 | string | Unique id for inter-element referencing | |||||
   |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
   |
Σ | 1..1 | uri | Identity of the terminology system | ||||
   |
Σ | 0..1 | string | Version of the system - if relevant | ||||
   |
Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
   |
Σ | 1..1 | string | Representation defined by the system | ||||
   |
Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
  |
SΣ | 0..1 | CodeableConcept | Specific type of encounter Binding: UK Core Encounter Type (required) | ||||
   |
0..1 | string | Unique id for inter-element referencing | |||||
   |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
   |
Σ | 0..* | Coding | Code defined by a terminology system | ||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
    |
Σ | 1..1 | uri | Identity of the terminology system | ||||
    |
Σ | 0..1 | string | Version of the system - if relevant | ||||
    |
Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
    |
Σ | 1..1 | string | Representation defined by the system | ||||
    |
Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
   |
Σ | 0..1 | string | Plain text representation of the concept | ||||
  |
SΣ | 0..1 | CodeableConcept | Specific type of service Binding: UK Core Care Setting Type (preferred): Any code from the SNOMED CT UK Refset with fully specified name 'Services simple reference set (foundation metadata concept)' with Refset Id 1127531000000102. | ||||
   |
0..1 | string | Unique id for inter-element referencing | |||||
   |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
   |
Σ | 0..* | Coding | Code defined by a terminology system | ||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
    |
Σ | 1..1 | uri | Identity of the terminology system | ||||
    |
Σ | 0..1 | string | Version of the system - if relevant | ||||
    |
Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
    |
Σ | 1..1 | string | Representation defined by the system | ||||
    |
Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
   |
Σ | 0..1 | string | Plain text representation of the concept | ||||
  |
S | 0..1 | CodeableConcept | Indicates the urgency of the encounter Binding: InterweaveEncounterPriority (required) | ||||
   |
0..1 | string | Unique id for inter-element referencing | |||||
   |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
   |
Σ | 0..* | Coding | Code defined by a terminology system | ||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
    |
Σ | 1..1 | uri | Identity of the terminology system | ||||
    |
Σ | 0..1 | string | Version of the system - if relevant | ||||
    |
Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
    |
Σ | 1..1 | string | Representation defined by the system | ||||
    |
Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
   |
Σ | 0..1 | string | Plain text representation of the concept | ||||
  |
SΣ | 1..1 | Reference(InterweavePatient) | The patient (NOT group) present at the encounter | ||||
   |
0..1 | string | Unique id for inter-element referencing | |||||
   |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
   |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
   |
Σ | 0..1 | uri | Type the reference refers to (e.g. "Patient") Binding: ResourceType (extensible): Aa resource (or, for logical models, the URI of the logical model). | ||||
   |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
   |
Σ | 1..1 | string | Description of the referenced resource | ||||
  |
Σ | 0..* | Reference(EpisodeOfCare) | Episode(s) of care that this encounter should be recorded against | ||||
  |
0..* | Reference(ServiceRequest) | The ServiceRequest that initiated this encounter | |||||
   |
0..1 | string | Unique id for inter-element referencing | |||||
   |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
   |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
   |
Σ | 0..1 | uri | Type the reference refers to (e.g. "Patient") Binding: ResourceType (extensible): Aa resource (or, for logical models, the URI of the logical model). | ||||
   |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
   |
Σ | 0..1 | string | If relevant, description of the referenced resource | ||||
  |
SΣ | 1..* | BackboneElement | The list of people responsible for providing the service. | ||||
   |
0..1 | string | Unique id for inter-element referencing | |||||
   |
0..* | Extension | Additional content defined by implementations | |||||
   |
?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
   |
SΣ | 1..1 | CodeableConcept | Role of participant in encounter Binding: ParticipantType (required) | ||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
    |
Σ | 0..* | Coding | Code defined by a terminology system | ||||
     |
0..1 | string | Unique id for inter-element referencing | |||||
     |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
     |
Σ | 1..1 | uri | Identity of the terminology system | ||||
     |
Σ | 0..1 | string | Version of the system - if relevant | ||||
     |
Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
     |
Σ | 1..1 | string | Representation defined by the system | ||||
     |
Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
    |
Σ | 0..1 | string | Plain text representation of the concept | ||||
   |
0..1 | Period | Period of time during the encounter that the participant participated | |||||
   |
SΣ | 1..1 | Reference(InterweavePractitioner) | Persons involved in the encounter other than the patient | ||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
    |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    |
Σ | 0..1 | uri | Type the reference refers to (e.g. "Patient") Binding: ResourceType (extensible): Aa resource (or, for logical models, the URI of the logical model). | ||||
    |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
    |
Σ | 1..1 | string | Description of the referenced resource | ||||
  |
SΣ | 0..1 | Reference(Appointment) | The appointment that scheduled this encounter | ||||
   |
0..1 | string | Unique id for inter-element referencing | |||||
   |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
   |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
   |
Σ | 0..1 | uri | Type the reference refers to (e.g. "Patient") Binding: ResourceType (extensible): Aa resource (or, for logical models, the URI of the logical model). | ||||
   |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
   |
Σ | 0..1 | string | If relevant, description of the referenced resource | ||||
  |
S | 1..1 | Period | The start and end time of the encounter | ||||
   |
0..1 | string | Unique id for inter-element referencing | |||||
   |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
   |
SΣC | 1..1 | dateTime | Starting time with inclusive boundary | ||||
   |
SΣC | 0..1 | dateTime | End time with inclusive boundary, if not ongoing | ||||
  |
0..1 | Duration | Quantity of time the encounter lasted (less time absent). Please use minutes. | |||||
  |
SΣ | 0..* | CodeableConcept | Reason the encounter takes place, expressed as a code. For admissions, this can be used for a coded admission diagnosis. Binding: EncounterReasonCodes (preferred): Reason why the encounter takes place. | ||||
   |
0..1 | string | Unique id for inter-element referencing | |||||
   |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
   |
Σ | 0..* | Coding | Code defined by a terminology system | ||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
    |
Σ | 1..1 | uri | Identity of the terminology system | ||||
    |
Σ | 0..1 | string | Version of the system - if relevant | ||||
    |
Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
    |
Σ | 1..1 | string | Representation defined by the system | ||||
    |
Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
   |
Σ | 0..1 | string | Plain text representation of the concept | ||||
  |
SΣ | 0..* | Reference(Condition | Procedure | Observation | ImmunizationRecommendation) | Reason the encounter takes place, expressed as a reference to a Condition, Procedure, Observation, or ImmunizationRecommendation. | ||||
  |
SΣ | 0..* | BackboneElement | The list of diagnosis relevant to this encounter Slice: Unordered, Open by value:use | ||||
   |
Content/Rules for all slices | |||||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations | |||||
    |
?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
    |
SΣ | 1..1 | Reference(Condition | Procedure) | The diagnosis or procedure relevant to the encounter | ||||
     |
0..1 | string | Unique id for inter-element referencing | |||||
     |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
     |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
     |
Σ | 0..1 | uri | Type the reference refers to (e.g. "Patient") Binding: ResourceType (extensible): Aa resource (or, for logical models, the URI of the logical model). | ||||
     |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
     |
Σ | 0..1 | string | If relevant, description of the referenced resource | ||||
    |
S | 1..1 | CodeableConcept | Role that this diagnosis has within the encounter (e.g. admission, billing, discharge …) Binding: DiagnosisRole (required) | ||||
     |
0..1 | string | Unique id for inter-element referencing | |||||
     |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
     |
Σ | 0..* | Coding | Code defined by a terminology system | ||||
      |
0..1 | string | Unique id for inter-element referencing | |||||
      |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
      |
Σ | 1..1 | uri | Identity of the terminology system | ||||
      |
Σ | 0..1 | string | Version of the system - if relevant | ||||
      |
Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
      |
Σ | 1..1 | string | Representation defined by the system | ||||
      |
Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
     |
Σ | 0..1 | string | Plain text representation of the concept | ||||
    |
S | 1..1 | positiveInt | Ranking of the diagnosis (for each role type) | ||||
   |
SΣ | 0..1 | BackboneElement | The list of diagnosis relevant to this encounter | ||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations | |||||
    |
?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
    |
Σ | 1..1 | Reference(Condition | Procedure) | The diagnosis or procedure relevant to the encounter | ||||
    |
0..1 | CodeableConcept | Role that this diagnosis has within the encounter (e.g. admission, billing, discharge …) Binding: DiagnosisRole (preferred): The type of diagnosis this condition represents. Fixed Value: As shown | |||||
     |
0..0 | string | Unique id for inter-element referencing | |||||
     |
0..0 | Extension | Additional content defined by implementations | |||||
     |
1..1 | Coding | Code defined by a terminology system Fixed Value: (complex) | |||||
      |
0..0 | string | Unique id for inter-element referencing | |||||
      |
0..0 | Extension | Additional content defined by implementations | |||||
      |
1..1 | uri | Identity of the terminology system Fixed Value: http://terminology.hl7.org/CodeSystem/diagnosis-role | |||||
      |
0..0 | string | Version of the system - if relevant | |||||
      |
1..1 | code | Symbol in syntax defined by the system Fixed Value: CC | |||||
      |
1..1 | string | Representation defined by the system Fixed Value: Chief complaint | |||||
      |
0..0 | boolean | If this coding was chosen directly by the user | |||||
     |
0..0 | string | Plain text representation of the concept | |||||
    |
0..1 | positiveInt | Ranking of the diagnosis (for each role type) | |||||
  |
S | 0..1 | BackboneElement | Details about the admission to a healthcare service | ||||
   |
0..1 | string | Unique id for inter-element referencing | |||||
   |
0..* | Extension | Extension Slice: Unordered, Open by value:url | |||||
    |
S | 0..1 | CodeableConcept | An extension to record how a patient was admitted to hospital URL: https://fhir.hl7.org.uk/StructureDefinition/Extension-UKCore-AdmissionMethod Binding: UK Core Admission Method (extensible): The method by which a patient was admitted to hospital | ||||
    |
S | 0..1 | (Complex) | Medically Safe for Discharge URL: https://fhir.interweavedigital.nhs.uk/R4/StructureDefinition/Extension-Interweave-MedicallySafeForDischarge | ||||
   |
?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
   |
0..1 | Identifier | Pre-admission identifier | |||||
   |
0..1 | Reference(Location | Organization) | The location from which the patient came before admission. Useful to provide if possible, in particular to reference a 'site' if transfered from another institution. | |||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
    |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    |
Σ | 0..1 | uri | Type the reference refers to (e.g. "Patient") Binding: ResourceType (extensible): Aa resource (or, for logical models, the URI of the logical model). | ||||
    |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
    |
Σ | 1..1 | string | Description of the referenced resource | ||||
   |
S | 0..1 | CodeableConcept | From where patient was admitted (physician referral, transfer) Binding: InterweaveAdmissionSource (required) | ||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
    |
Σ | 0..* | Coding | Code defined by a terminology system | ||||
     |
0..1 | string | Unique id for inter-element referencing | |||||
     |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
     |
Σ | 1..1 | uri | Identity of the terminology system | ||||
     |
Σ | 0..1 | string | Version of the system - if relevant | ||||
     |
Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
     |
Σ | 1..1 | string | Representation defined by the system | ||||
     |
Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
    |
Σ | 0..1 | string | Plain text representation of the concept | ||||
   |
0..1 | CodeableConcept | The type of hospital re-admission that has occurred (if any). If the value is absent, then this is not identified as a readmission Binding: hl7VS-re-admissionIndicator (example): The reason for re-admission of this hospitalization encounter. | |||||
   |
0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing Binding: Diet (example): Medical, cultural or ethical food preferences to help with catering requirements. | |||||
   |
0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing Binding: SpecialCourtesy (preferred): Special courtesies. | |||||
   |
0..* | CodeableConcept | DISCOURAGED: Relevant for managing the patient's stay, but less so for regional sharing Binding: SpecialArrangements (preferred): Special arrangements. | |||||
   |
S | 0..1 | Reference(Location | Organization) | Location to which the patient is discharged. Important to provide if known to support discharge planning, and/or to reference a 'site' if transfered to another institution. | ||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
    |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    |
Σ | 0..1 | uri | Type the reference refers to (e.g. "Patient") Binding: ResourceType (extensible): Aa resource (or, for logical models, the URI of the logical model). | ||||
    |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
    |
Σ | 1..1 | string | Description of the referenced resource | ||||
   |
S | 0..1 | CodeableConcept | Category or kind of location after discharge Binding: InterweaveDischargeDestination (required) | ||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
    |
Σ | 0..* | Coding | Code defined by a terminology system | ||||
     |
0..1 | string | Unique id for inter-element referencing | |||||
     |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
     |
Σ | 1..1 | uri | Identity of the terminology system | ||||
     |
Σ | 0..1 | string | Version of the system - if relevant | ||||
     |
Σ | 1..1 | code | Symbol in syntax defined by the system | ||||
     |
Σ | 1..1 | string | Representation defined by the system | ||||
     |
Σ | 0..1 | boolean | If this coding was chosen directly by the user | ||||
    |
Σ | 0..1 | string | Plain text representation of the concept | ||||
  |
S | 0..* | BackboneElement | Location the encounter takes place (at Ward level) | ||||
   |
0..1 | string | Unique id for inter-element referencing | |||||
   |
0..* | Extension | Additional content defined by implementations | |||||
   |
?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
   |
S | 1..1 | Reference(Location) | Location the encounter takes place | ||||
    |
0..1 | string | Unique id for inter-element referencing | |||||
    |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
    |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
    |
Σ | 0..1 | uri | Type the reference refers to (e.g. "Patient") Binding: ResourceType (extensible): Aa resource (or, for logical models, the URI of the logical model). | ||||
    |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
    |
Σ | 1..1 | string | Description of the referenced resource | ||||
   |
S | 1..1 | code | planned | active | reserved | completed Binding: EncounterLocationStatus (required): The status of the location. | ||||
   |
0..1 | CodeableConcept | The physical type of the location (usually the level in the location hierachy - bed room ward etc.) Binding: UK Core Encounter Location Type (preferred): A set of codes that define the physical type of location where an encounter takes place. | |||||
   |
S | 1..1 | Period | Time period during which the patient was present at the location | ||||
  |
0..1 | Reference(Organization) | DISCOURAGED: This is instead covered via the provenance tags | |||||
  |
0..1 | Reference(InterweaveEncounterGrouping) | Another Encounter this encounter is part of | |||||
   |
0..1 | string | Unique id for inter-element referencing | |||||
   |
0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
   |
ΣC | 1..1 | string | Reference to a resource (could be Contained) | ||||
   |
Σ | 0..1 | uri | Type the reference refers to (e.g. "Patient") Binding: ResourceType (extensible): Aa resource (or, for logical models, the URI of the logical model). | ||||
   |
Σ | 0..1 | Identifier | If relevant could include an id | ||||
   |
Σ | 0..1 | string | If relevant, description of the referenced resource | ||||
 Documentation for this format Documentation for this format | ||||||||
| Path | Conformance | ValueSet / Code | URI | |||
| Encounter.meta.security | extensible | All Security Labelshttp://hl7.org/fhir/ValueSet/security-labelsfrom the FHIR Standard | ||||
| Encounter.meta.tag | example | CommonTagshttp://hl7.org/fhir/ValueSet/common-tagsfrom the FHIR Standard | ||||
| Encounter.meta.tag:Source | example | CommonTagshttp://hl7.org/fhir/ValueSet/common-tagsfrom the FHIR Standard | ||||
| Encounter.meta.tag:Provenance | example | CommonTagshttp://hl7.org/fhir/ValueSet/common-tagsfrom the FHIR Standard | ||||
| Encounter.language | preferred | CommonLanguages
http://hl7.org/fhir/ValueSet/languagesfrom the FHIR Standard | ||||
| Encounter.identifier.use | required | IdentifierUsehttp://hl7.org/fhir/ValueSet/identifier-use|4.0.1from the FHIR Standard | ||||
| Encounter.identifier.type | extensible | Identifier Type Codeshttp://hl7.org/fhir/ValueSet/identifier-typefrom the FHIR Standard | ||||
| Encounter.identifier:localIdentifier.use | required | IdentifierUsehttp://hl7.org/fhir/ValueSet/identifier-use|4.0.1from the FHIR Standard | ||||
| Encounter.identifier:localIdentifier.type | extensible | Identifier Type Codeshttp://hl7.org/fhir/ValueSet/identifier-typefrom the FHIR Standard | ||||
| Encounter.status | required | EncounterStatushttp://hl7.org/fhir/ValueSet/encounter-status|4.0.1from the FHIR Standard | ||||
| Encounter.statusHistory.status | required | EncounterStatushttp://hl7.org/fhir/ValueSet/encounter-status|4.0.1from the FHIR Standard | ||||
| Encounter.class | required | InterweaveEncounterClasshttps://fhir.interweavedigital.nhs.uk/R4/ValueSet/Interweave-EncounterClassfrom this IG | ||||
| Encounter.classHistory.class | extensible | ActEncounterCodehttp://terminology.hl7.org/ValueSet/v3-ActEncounterCode | ||||
| Encounter.type | required | UKCoreEncounterTypehttps://fhir.hl7.org.uk/ValueSet/UKCore-EncounterTypefrom this IG | ||||
| Encounter.serviceType | preferred | UKCoreCareSettingTypehttps://fhir.hl7.org.uk/ValueSet/UKCore-CareSettingTypefrom this IG | ||||
| Encounter.priority | required | InterweaveEncounterPriorityhttps://fhir.interweavedigital.nhs.uk/R4/ValueSet/Interweave-EncounterPriorityfrom this IG | ||||
| Encounter.subject.type | extensible | ResourceTypehttp://hl7.org/fhir/ValueSet/resource-typesfrom the FHIR Standard | ||||
| Encounter.basedOn.type | extensible | ResourceTypehttp://hl7.org/fhir/ValueSet/resource-typesfrom the FHIR Standard | ||||
| Encounter.participant.type | required | ParticipantTypehttp://hl7.org/fhir/ValueSet/encounter-participant-typefrom the FHIR Standard | ||||
| Encounter.participant.individual.type | extensible | ResourceTypehttp://hl7.org/fhir/ValueSet/resource-typesfrom the FHIR Standard | ||||
| Encounter.appointment.type | extensible | ResourceTypehttp://hl7.org/fhir/ValueSet/resource-typesfrom the FHIR Standard | ||||
| Encounter.reasonCode | preferred | EncounterReasonCodeshttp://hl7.org/fhir/ValueSet/encounter-reasonfrom the FHIR Standard | ||||
| Encounter.diagnosis.condition.type | extensible | ResourceTypehttp://hl7.org/fhir/ValueSet/resource-typesfrom the FHIR Standard | ||||
| Encounter.diagnosis.use | required | DiagnosisRolehttp://hl7.org/fhir/ValueSet/diagnosis-rolefrom the FHIR Standard | ||||
| Encounter.diagnosis:chiefComplaint.use | preferred | Fixed Value: CC("Chief complaint")http://hl7.org/fhir/ValueSet/diagnosis-rolefrom the FHIR Standard | ||||
| Encounter.hospitalization.origin.type | extensible | ResourceTypehttp://hl7.org/fhir/ValueSet/resource-typesfrom the FHIR Standard | ||||
| Encounter.hospitalization.admitSource | required | InterweaveAdmissionSourcehttps://fhir.interweavedigital.nhs.uk/R4/ValueSet/Interweave-AdmissionSourcefrom this IG | ||||
| Encounter.hospitalization.reAdmission | example | Hl7VSReAdmissionIndicatorhttp://terminology.hl7.org/ValueSet/v2-0092 | ||||
| Encounter.hospitalization.dietPreference | example | Diethttp://hl7.org/fhir/ValueSet/encounter-dietfrom the FHIR Standard | ||||
| Encounter.hospitalization.specialCourtesy | preferred | SpecialCourtesyhttp://hl7.org/fhir/ValueSet/encounter-special-courtesyfrom the FHIR Standard | ||||
| Encounter.hospitalization.specialArrangement | preferred | SpecialArrangementshttp://hl7.org/fhir/ValueSet/encounter-special-arrangementsfrom the FHIR Standard | ||||
| Encounter.hospitalization.destination.type | extensible | ResourceTypehttp://hl7.org/fhir/ValueSet/resource-typesfrom the FHIR Standard | ||||
| Encounter.hospitalization.dischargeDisposition | required | InterweaveDischargeDestinationhttps://fhir.interweavedigital.nhs.uk/R4/ValueSet/Interweave-DischargeDestinationfrom this IG | ||||
| Encounter.location.location.type | extensible | ResourceTypehttp://hl7.org/fhir/ValueSet/resource-typesfrom the FHIR Standard | ||||
| Encounter.location.status | required | EncounterLocationStatushttp://hl7.org/fhir/ValueSet/encounter-location-status|4.0.1from the FHIR Standard | ||||
| Encounter.location.physicalType | preferred | UKCoreEncounterLocationTypehttps://fhir.hl7.org.uk/ValueSet/UKCore-EncounterLocationTypefrom this IG | ||||
| Encounter.partOf.type | extensible | ResourceTypehttp://hl7.org/fhir/ValueSet/resource-typesfrom the FHIR Standard |
| Id | Grade | Path(s) | Details | Requirements |
| dom-2 | error | Encounter | If the resource is contained in another resource, it SHALL NOT contain nested Resources : contained.contained.empty() | |
| dom-3 | error | Encounter | If the resource is contained in another resource, it SHALL be referred to from elsewhere in the resource or SHALL refer to the containing resource : contained.where((('#'+id in (%resource.descendants().reference | %resource.descendants().as(canonical) | %resource.descendants().as(uri) | %resource.descendants().as(url))) or descendants().where(reference = '#').exists() or descendants().where(as(canonical) = '#').exists() or descendants().where(as(canonical) = '#').exists()).not()).trace('unmatched', id).empty() | |
| dom-4 | error | Encounter | If a resource is contained in another resource, it SHALL NOT have a meta.versionId or a meta.lastUpdated : contained.meta.versionId.empty() and contained.meta.lastUpdated.empty() | |
| dom-5 | error | Encounter | If a resource is contained in another resource, it SHALL NOT have a security label : contained.meta.security.empty() | |
| dom-6 | best practice | Encounter | A resource should have narrative for robust management : text.`div`.exists() | |
| ele-1 | error | **ALL** elements | All FHIR elements must have a @value or children : hasValue() or (children().count() > id.count()) | |
| ext-1 | error | **ALL** extensions | Must have either extensions or value[x], not both : extension.exists() != value.exists() |
This structure is derived from UKCoreEncounter
Summary
Mandatory: 13 elements(46 nested mandatory elements)
Must-Support: 40 elements
Fixed: 4 elements
Prohibited: 8 elements
Structures
This structure refers to these other structures:
Extensions
This structure refers to these extensions:
Slices
This structure defines the following Slices:
Other representations of profile: CSV, Excel, Schematron
| Element name | Change details |
|---|---|
| extension:dischargeMethod |
|
| extension:encounterTransport |
|
| extension:emergencyCareDischargeDestination |
|
| extension:emergencyCareDischargeStatus |
|
| extension:legalStatus |
|
| extension:outcomeOfAttendance |
|
| extension:serviceType |
|
| identifier:localIdentifier.system |
|
| class |
|
| type |
|
| serviceType |
|
| priority |
|
| basedOn |
|
| reasonCode |
|
| reasonReference |
|
| diagnosis.use |
|
| diagnosis.condition |
|
| hospitalization.extension:dischargeMethod |
|
| hospitalization.extension:admissionMethod |
|
| hospitalization.extension:medicallySafeForDischarge |
|
| hospitalization.extension:medicallySafeForDischarge.extension:status |
|
| hospitalization.origin |
|
| hospitalization.admitSource |
|
| hospitalization.destination |
|
| hospitalization.dischargeDisposition |
|
| location.physicalType |
|